Cutaneous metastasis of renal cell carcinoma through percutaneous fine needle aspiration biopsy: Case report
Published Web Location
https://doi.org/10.5070/D38m16x0j6Main Content
Cutaneous metastasis of renal cell carcinoma through percutaneous fine needle aspiration biopsy: Case report
Ghorbel Jilani1, Dridi Mohamed1, Hellara Wadia1, Khiari Ramzi1, Jones Meriem2, Laarbi Houssem1, Ghozzi Samir1, Ben Raies Nawfel1
Dermatology Online Journal 16 (2): 10
1. Urology Department, Militairy Hospital of Tunis, 1008, Monfleury, Tunis, Tunisia. ghorbeljilani@yahoo.fr2. Service de Dermatologie, Hôpital Militaire Principal d’Instructions de Tunis, 1008, Monfleury, Tunis, Tunisia
Abstract
A 39-year-old man, who had undergone left nephrectomy for renal cell carcinoma of clear cell type, was noted to have a solitary nodular shadow in the right lung on chest X-ray. Percutaneous needle biopsy of the lung was performed via the right anterior chest wall and the histologic findings showed metastasis from renal carcinoma. Six month later, the patient presented with a cutaneous nodule at the site of puncture of the lung needle biopsy. Histological examination of a biopsy of the skin tumor revealed features of metastatic renal cell carcinoma of clear cell type. Surgical excision of the cutaneous nodule was performed, followed by radiotherapy at the site of the skin lesion on the chest wall. After treatment, the patient remains disease free after one year of follow-up. This case represents an unusual clinical presentation of metastatic renal cell carcinoma that appears to have been translocated to the skin by the needle biopsy.
Introduction
The risk of the emergence of pulmonary metastasis of renal carcinoma after surgery has been estimated between 30 and 40 percent, with average delay of 15 months [1]. Thus to confirm the renal neoplasia origin of a pulmonary mass, percutaneous fine-needle aspiration biopsy (FNAB) is often used. Although it is a useful diagnostic procedure, various complications, such as pneumothorax, bleeding, infection, air embolism, and implantation metastasis, have been reported [2, 3]. However, implantation of malignant cells along the needle tract is an extremely rare complication after FNAB, which can change a potentially resectable localized lung metastsis to an unresectable carcinoma. We present a case of pulmonary metastasis from renal carcinoma with subcutaneous implantation of tumor cells along the needle tract after percutaneous needle biopsy of the lung.
Observation
 |  |
| Figure 1 | Figure 2 |
|---|---|
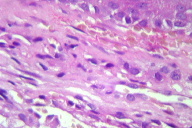
| Figure 1. Well-circumscribed violaceous nodule 2 cm in diameter Figure 2. Histologic examination showing metastatic renal cell carcinoma of clear cell type (H&E, x20) | |
A 39-year-old man had undergone left radical nephrectomy for renal carcinoma. The initial TNM staging of the renal tumor was T2 Nx M0. Histological examination of the surgical specimen revealed clear cell renal carcinoma pT2 N0. After 6 months, the patient was noted to have a solitary nodule in the right lung on chest X-ray. The chest computed tomogram showed a nodular mass in the peripheral lower part of the right lung. Fiberbronchoscopy was normal. Percutaneous fine needle aspiration biopsy of the lung via the right anterior chest wall, using a 20 gauge fine needle, showed metastasis from renal cell carcinoma. The patient was treated with immunotherapy with subcutaneous interferon injections. After six months, he presented with a well-circumscribed, hard, violaceous nodule, 2 cm in diameter, at the site of puncture of the lung needle biopsy (Figure 1). Histological examination of a skin biopsy of the cutaneous nodule revealed features of metastasis from renal cell carcinoma of clear cell type (Figure 2). Surgical excision of the cutaneous tumor was performed, followed by radiotherapy at the site of the skin lesion on the chest wall. After futher immunotherapy, he remains disease free after one year of follow-up.
Discussion
The lung is one of the most frequently affected metastatic sites in patients with renal cell carcinoma. Nearly 30 percent of all patients with renal cell carcinoma will eventually present with metastatic disease after radical nephrectomy. Many reports suggest a role for pulmonary metastasectomy in managing metastatic renal cell carcinoma [1].
As fine-needle aspiration biopsy is a simple and easy procedure with high sensitivity and low mortality, it is often used to diagnose lung disease. Although the incidence of complication in fine-needle aspiration biopsy is reported to be low, various complications, such as pneumothorax, infection, bleeding, air embolism, and implantation metastasis [2, 3] have been reported. Tumor dissemination in the needle tract is a rare complication [4]. Larger series have estimated that the incidence of this complication is less than 1 percent. However, the total number of biopsies in these series included patients with benign disease and patients with multiple procedures whose needle biopsies had been nondiagnostic [5]. In addition, case reports have been limited to patients who have evidence of disease in the chest wall. Thus, current estimates do not include cases of pleural dissemination, subclinical disease, or patients who were lost to follow-up or died of unrelated diseases before local spread was identified. In addition, the incidence of implantation metastasis is relatively high when the cell type is an adenocarcinoma or when a large bore needle is used. However, tumor-seeding has also been described when fine needles smaller than 22-gauge are used, as in our case [6]. In order to avoid this devastating complication, the needle should be smaller than 21-gauge and the biopsy should be localized to a single entrance rather than multiple. Many authors recommend using a biopsy needle that comes with a covering sheath so that the needle is withdrawn into the sheath first before removing it from the patient in order to preclude direct cancer seeding into the chest wall, which is the main cause of chest wall implantation. As a general practice, we use 22-gauge needles for aspiration biopsies and 19.5-gauge needles for gun biopsies. Although Sawabata et al. suggested that tumor cells remaining in the pleural space after PTNB in a tumor model might cause pleural carcinomatosis and could grow, The clinical implication of these findings is unknown [7]. Struve-Christensen showed that malignant cells could be found in a high percentage of needle biopsy tracks but this produced a clinically significant lesion in a minority of cases [8].
Previous case reports have demonstrated that the duration of implantation metastasis after needle aspiration varies from 6 months to 26 months. It should be stressed that a high index of suspicion is necessary for early diagnosis and that a careful physical examination of the needle biopsy site is mandatory during the follow-up periods.
However, different studies show that although PTNB is a cause of concern [9, 10], it is not sufficient to contraindicate the use of this procedure. Moreover the study of Juan P. et al. [11] shows that preoperative PTNB is not associated with increased risk of mortality among patients with localized non-small cell lung cancer. Thus, lung cancer dissemination does not appear to be a common phenomenon among these patients. This information should reassure physicians considering the use of this procedure for the work-up of solitary pulmonary nodules when there is a suspicion of lung cancer because early detection is essential. This means that the treating physician must be aware of all aspects of this subject and be suspicious of the existence of such metastases in patients who have undergone the procedure.
The treatment strategy for implantation metastasis is controversial. Seyfer et al. suggested that a wide en-bloc excision and a muscular or musculocutaneous flap must be used if there is no evidence of distant metastasis [4]. Postoperative local radiation therapy can be associated with a usual palliative dose of 4000-5000 Gy [12].
Conclusion
The risk of implantation metastasis after PNAB is real, but this possibility of implantation metastasis should not be used as an argument against the use of PCNB when required. Implantation metastasis can be minimized by using a small bore needle and managed by wide excision and postoperative radiation therapy. If implantation metastasis is found early so that the nodule is small in size, the result of the surgical resection is acceptable. Thus, physicians and dermatologists following up patients who have undergone PCNB should always be awareness of the possibility of implantation metastasis after this procedure.
References
1. Chen F, Fujinaga T, Shoji T, Miyahara R, Bando T, Okubo K, Hirata T, Date H. Pulmonary resection for metastasis from renal cell carcinoma. Interact Cardiovasc Thorac Surg. 2008 Oct;7(5):825-8. [PubMed]2. Voravud N, Shin DM, Dekmezian RH, Dimery I, Lee JS, Hong WK. Implantation metastasis of carcinoma after percutaneous fine-needle aspiration biopsy. Chest. 1992 Jul;102(1):313-5. [PubMed]
3. Dick R, Heard BE, Hinson KF, Kerr IH, Pearson MC. Aspiration needle biopsy of thoracic lesions: an assessment of 227 biopsies. Br J Dis Chest. 1974 Apr;68(2):86-94. [PubMed]
4. Seyfer AE, Walsh DS, Graeber GM, Nuno IN, Eliasson AH. Chest wall implantation of lung cancer after thin-needle aspiration biopsy. Ann Thorac Surg. 1989 Aug;48(2):284-6. [PubMed]
5. Kim JH, Kim YT, Lim HK, Kim YH, Sung SW. Management for chest wall implantation of non-small cell lung cancer after fine-needle aspiration biopsy. Eur J Cardiothorac Surg. 2003 May;23(5):828-32. [PubMed]
6. McDonald CF, Baird L. Risk of needle track metastasis after fine needle lung aspiration in lung cancer--a case report. Respir Med. 1994 Sep;88(8):631-2. [PubMed]
7. Sawabata N, Ohta M, Maeda H. Fine-needle aspiration cytologic technique for lung cancer has a high potential of malignant cell spread through the tract. Chest. 2000 Oct;118(4):936-9. [PubMed]
8. Wolinsky H, Lischner MW. Needle track implantation of tumor after percutaneous lung biopsy. Ann Intern Med. 1969 Aug;71(2):359-62. [PubMed]
9. Hix WR, Aaron BL. Needle aspiration in lung cancer. Risk of tumor implantation is not negligible. Chest. 1990 Mar;97(3):516-7. [PubMed]
10. Kara M, Alver G, Sak SD, Kavukçu S. Implantation metastasis caused by fine needle aspiration biopsy following curative resection of stage IB non-small cell lung cancer. Eur J Cardiothorac Surg. 2001 Oct;20(4):868-70. [PubMed]
11. Wisnivesky JP, Henschke CI, Yankelevitz DF. Diagnostic percutaneous transthoracic needle biopsy does not affect survival in stage I lung cancer. Am J Respir Crit Care Med. 2006 Sep 15;174(6):684-8. [PubMed]
12. Abratt RP, Willcox PA. The effect of irradiation on lung function and perfusion in patients with lung cancer. Int J Radiat Oncol Biol Phys. 1995 Feb 15;31(4):915-9. [PubMed]
© 2010 Dermatology Online Journal

