Umbilical basal cell carcinoma in a 21-year-old man: Report of an exceptional case and dermatoscopic evaluation
Published Web Location
https://doi.org/10.5070/D36jm8h8mgMain Content
Letter: Umbilical basal cell carcinoma in a 21-year-old man: Report of an exceptional case and dermatoscopic evaluation
Paloma Ramirez MD, Elena Sendagorta MD, Marta Feito MD, Maria Gonzalez-Beato MD, Matias Mayor PhD, Angel Pizarro PhD
Dermatology Online Journal 17 (1): 16
H. Universitario La Paz, Madrid, Spain. palomarm@gmail.comAbstract
We report an exceptional case of umbilical basal cell carcinoma (BCC) in a 21-year-old man, whose correct diagnosis was suggested by dermoscopy during initial complete body mole mapping. Although BCC is a common skin tumor, only 7 cases of BCC arising within the umbilicus have been reported previously. To the best of our knowledge, our patient is unique because of his age, being the youngest case of umbilical BCC described in the literature. Complete examination and digital dermoscopic monitoring let us identify an asymptomatic, nonpigmented papule at the umbilicus. Dermoscopy images revealed signs of superficial ulceration and several types of vascular structures, which gave us the clue for the diagnosis and helped us differentiate it from other lesions such as Spitz nevus or amelanotic melanoma. The diagnosis was confirmed with histopathology after excision and there was no evidence of relapse in the following four years.
Introduction
Basal cell carcinoma (BCC) occurs predominantly on sun-exposed skin. BCC arising de novo within the umbilicus is exceedingly rare, with only 7 cases reported previously in the literature (Table 1) [1-6]. Dermoscopy is a noninvasive diagnostic technique that is known to improve accuracy in the diagnosis of pigmented lesions and non-pigmented skin tumors, for which the clinical diagnosis is often uncertain. In this situation, the recognition of distinctive vascular structures may be of primary importance, as it has been demonstrated in our case [7, 8, 9].
Case synopsis
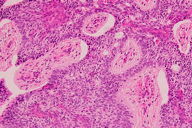
A 21-year-old man with skin phototype II and multiple atypical melanocytic nevi was being followed in our pigmented lesion unit. The predominant nevus type in this patient was a flat lesion with homogeneous light-brown or pink coloration and minimal pigmented structures on dermoscopy (Figure 1a). In this clinical context early diagnosis of amelanotic melanoma may be difficult, which prompted us to use digital dermoscopic monitoring for follow-up. During initial complete body mole mapping, a small umbilical pink-colored papule was identified (Figure 1b). The papule was asymptomatic and it had gone unnoticed by the patient up to that moment. Despite being clinically non-specific and unpigmented, dermoscopy images exhibited a semi-translucent appearance with signs of small superficial ulceration and various types of vascular structures. These included hairpin vessels, fine elongated telangiectasias, and some prominent arborizing vessels, perfectly in focus in the image (Figure 1c) [10]. The dermatoscopic findings were suggestive of BCC and the diagnosis was confirmed by histopathology after excision (Figure 2). The surgical defect was reconstructed with a rotation flap; there was no evidence of recurrence after four years of follow-up (Figure 1d). The patient denied having any skin trauma, prior surgical procedures, or chronic inflammation at the umbilicus. Interestingly, his father had developed a BCC that was excised from his back at the age of 48. He also was diagnosed with a testicular seminoma at age 42, but there were no other personal or family clinical data to suggest the potential diagnosis of a cancer-related genodermatosis, such as Gorlin-Goltz syndrome or xeroderma pigmentosum. A panoramic Xray (PANOREX) was taken to rule out the presence of odontogenic jaw cysts, frequently found in Gorlin-Goltz syndrome, and there were no abnormalities.
BCC is the most frequent cutaneous malignancy in the light-skinned population worldwide. The large majority of BCCs arise around the head and neck, but they may occur at other sites, including the abdomen. Primary malignant tumors occurring at the umbilicus are unusual and a review of the literature revealed only a few reports of umbilical BCC. Malignancy at the umbilical area is usually a metastasis, most often from the gastrointestinal tract, but primary skin lesions both benign and malignant should be considered in the differential diagnosis. The high incidence of non-melanoma skin cancer in white populations has prompted a few reports on the relationship with non-cutaneous cancer. We must emphasize that our patient’s father had developed both a testicular seminoma and a BCC. Frisch et al reported that in addition to having an increased risk for new skin cancer, patients with BCC have an increased risk for non-cutaneous cancer at various sites, including testicular cancer, particularly for patients in whom BCC is diagnosed before 60 years of age [11]. We postulate that polymorphisms in some unknown low-penetrance cancer-related genes could have favored the presence of seminoma and BCC in his father and the early onset of BCC within the umbilicus in our patient. Additionally, various authors have suggested some unique characteristics of truncal BCC [3, 12]. Interestingly, it frequently develops in younger patients and more often in men than in women. Truncal BCCs also tend to grow larger and are associated with an increased risk for developing multiple non-melanoma skin cancers. This increased risk has been attributed to genetic susceptibility UV-induced oxidative damage in the skin.
The clinical diagnosis of BCC may not always be easy and dermoscopy has been demonstrated to improve diagnostic accuracy. Dermoscopy, as an adjunct to the clinical examination, was found to be a useful tool for diagnosing both pigmented and non-pigmented skin lesions because it permits, besides the pigmented structures, the recognition of specific vascular structures [7, 8, 9]. Therefore, lacking any pigmented structure, the vascular morphologies found in the dermoscopic image gave us the clues to the diagnosis and helped us differentiate it from potentially confounding lesions like Spitz nevus or even amelanotic melanoma.
Finally, the patient underwent surgery without any complication. Nevertheless, therapeutic management of umbilical BCCs may be difficult if lesions are infiltrative or large in size. In those cases, although wide local excision remains the most commonly used treatment, Mohs micrographic surgery should be considered. Moreover, we must highlight the exceptional anatomy of the umbilicus; its close proximity to various anatomic structures may facilitate tumor spread.
In conclusion, we have reported an exceptional case of BCC not only for its atypical location but also for the patient’s age. To the best of our knowledge, this is the youngest case reported of BCC arising at the umbilicus.
References
1. Chuang GS, Lu LK, Finn D. Basal cell carcinoma invading the umbilical stalk excised with Mohs micrographic surgery: case report and review of umbilical anatomy. Dermatol Surg. 2009 Aug;35(8):1290-3. Epub 2009 May 12. Review. [PubMed]2. Durrani AJ, Miller RJ, Davies M. Basal cell carcinoma arising in a laparoscopic port site scar at the umbilicus. Plast Reconstr Surg. 2005 Jul;116(1):348-50. [PubMed]
3. Etter L, Cook JL. Basal cell carcinoma of the umbilicus: a case report and literature review. Cutis. 2003 Feb;71(2):123-6. Review. [PubMed]
4. Walker SL, Banerjee P, Marsden RA. Basal cell carcinoma arising at the umbilicus. Clin Exp Dermatol. 2001 Jul;26(5):458-9. [PubMed]
5. Schneider HJ, Young AE. Sister Joseph's nodule. Eur J Surg Oncol. 1998 Apr;24(2):155. [PubMed]
6. Steck WD, Helwig EB. Tumors of the umbilicus. Cancer. 1965 Jul;18:907-15. [PubMed]
7. Argenziano G, Zalaudek I, Corona R, Sera F, Cicale L, Petrillo G, Ruocco E, Hofmann-Wellenhof R, Soyer HP. Vascular structures in skin tumors: a dermoscopy study. Arch Dermatol. 2004 Dec;140(12):1485-9. [PubMed]
8. Zalaudek I, Kreusch J, Giacomel J, Ferrara G, Catricalà C, Argenziano G. How to diagnose nonpigmented skin tumors: a review of vascular structures seen with dermoscopy: part I. Melanocytic skin tumors. J Am Acad Dermatol. 2010 Sep;63(3):361-74. [PubMed]
9. Zalaudek I, Kreusch J, Giacomel J, Ferrara G, Catricalà C, Argenziano G. How to diagnose nonpigmented skin tumors: a review of vascular structures seen with dermoscopy: part II. Nonmelanocytic skin tumors. J Am Acad Dermatol. 2010 Sep;63(3):377-86. [PubMed]
10. Stoecker WV, Kolm I, Rabinovitz HS, Oliviero MC, Xu J, Malters JM. Semitranslucency in dermoscopic images of basal cell carcinoma. Arch Dermatol. 2009 Feb;145(2):224. [PubMed]
11. Frisch M, Hjalgrim H, Olsen JH, Melbye M. Risk for subsequent cancer after diagnosis of basal-cell carcinoma. A population-based, epidemiologic study. Ann Intern Med. 1996 Nov 15;125(10):815-21. [PubMed]
12. Neale RE, Davis M, Pandeya N, Whiteman DC, Green AC. Basal cell carcinoma on the trunk is associated with excessive sun exposure. J Am Acad Dermatol. 2007 Mar;56(3):380-6. [PubMed]
© 2011 Dermatology Online Journal