Chromomycosis arising in a Tunisian man
Published Web Location
https://doi.org/10.5070/D36ff7t5x6Main Content
Chromomycosis arising in a Tunisian man
N Ezzine-Sebaï1 MD, R Benmously1 MD, B Fazaa1 MD E Chaker2 MD, R Zermani3 MD, and MR Kamoun1MD
Dermatology Online Journal 11 (2): 14
1. Dermatology department Charles Nicolle Hospital. rym.benmously@rns.tn2. Parasitology department La Rabta hospital 3. Anatomo-pathology
department Charles Nicolle Hospital- Tunis-Tunisia
Abstract
Chromomycosis is a chronic fungal infection quite prevalent in tropical countries. In such areas, it has a chronic evolutional course that may cause several problems. In our country, this disorder is quite rare. Herein we report the second case of Tunisian chromoblastomycosis. A-28-year-old man from north Tunisia (Bizerte) presented to our dermatology department with a skin lesion of 1½ years duration. He was a butcher leaving in a rural area. The lesion gradually expanded to form a 3.5-cm violet-colored tumor with a verrucous surface. The tumor was located in the patient's left buttock. Scraping from the border of the lesion was negative. Cultures grew Fonsecaea pedrosoi. The lesion was surgically removed and the patient was treated with oral terbinafine (500 mg/day) for 2 months. There was no recurrence within a followup period of 3 years. Chromomycosis is a slowly progressive cutaneous mycosis caused by various dematiceous fungi prevalent in tropical countries. In Tunisia, this disease is rarely encountered. Dermatologists should be aware of this diagnosis. For limited lesions, we recommend excision followed by oral terbinafine.
Chromomycosis (chromoblastomycosis) is a chronic fungal infection prevalent in tropical regions. This condition has a chronic evolutional course that may be associated with development of epidermoid carcinoma.
Chromomycosis is quite rare in Tunisia, and can cause some diagnostic difficulties. We report the second case of Tunisian chromomycosis.
Clinical synopsis

|
|
| Figure 1 | Figure 2 |
|---|---|
| Figure 1: A violet-colored tumor of 3.5 cm with a verrucous surface on the left buttock. | |
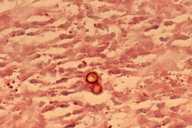
| Figure 2: Fungal cells are present within chromoblastomycosis granuloma. | |

|
| Figure 3a |
|---|
| Fonsecaea pedrosoi: Colony aspect on culture tube. |
A 28-year-old healthy man from north Tunisia (Bizerte) presented to our dermatology department with a skin lesion of 1½ years duration. He was a butcher living in a rural area.

|

|
| Figure 3b | Figure 3c |
|---|---|
| Hormondentron short form (Fig. 3b) | |
| Acrotheca form (Fig. 3c) | |
The lesion gradually expanded to form a 3.5-cm violet-colored tumor with a verrucous surface. The tumor was located in the patient's left buttock (Fig. 1). The diagnosis of cutaneous leishmaniasis was suspected, but scraping from the border of the lesion was negative for leishmaniasis. A biopsy specimen revealed the presence of fungal elements within a granulomatous reaction (Fig. 2). Cultures grew Fonsecaea pedrosoi (Figs. 3a, 3b, 3c).
The chest X ray and biological tests were within normal limits.
There was no evidence of any immunodeficiency. The lesion was surgically removed and the patient was treated with oral terbinafine (500 mg/day) for 2 months. There was no recurrence within a 3-year followup period.
Discussion
Chromomycosis is a slowly progressive cutaneous mycosis caused by various dematiaceous fungi prevalent in tropical and humid countries. Major endemic areas include Madagascar [1], some islands of the Indian Ocean, South Africa, Asia, the Caribbean and Amazonian areas. Chromomycosis is attributed to several different dematiaceous fungi, including phialophora, cladosporium, Wangiella, and Fonsecaeca, as well as a few other genera anecdotally found in the literature [2]. These agents are found worldwide in soil and in decaying plant materials, including wood.
In the Maghreb countries, chromomycosis is rare. Among 30 observations of deep mycoses in Morocco, only 5 patients presented chromomycosis [3]. In Algeria, chromomycosis was first described by Perrin et al. in 1989 [4]. Subsequently, seven cases have been reported [5]. In Tunisia, this disease is rarely encountered. There is only one previous report, published in 2002, involving a woman living in a rural area [6].
The primary lesion is thought to develop as a result of percutaneous traumatic inoculation. From the site of inoculation, the lesion usually restricts itself to cutaneous and subcutaneous tissue, especially in parts of the body not protected by clothing.
The disease affects predominantly men. Typical lesions grow slowly over many years and tend to be found on the lower limbs. According to Minotto R et al., 27 percent of the cases involve other areas, including the medial canthus of the eye, the ear, neck, shoulder, chest, wrist and buttocks [7]. The morphology of the lesion may be tumor (as in our patient), nodular, verrucous, plaque-like, psoriasiform, or scar [2, 8]. Our patient worked as a butcher and trauma was frequent. However, his lesion occurred curiously in a covered area.
In our country chromomycosis lesions may be confused with leishmaniasis, verrucous tuberculosis, and tertiary syphilis. Scraping from a verrucous lesion in potassium hydroxide preparation reveals mycelia arising from sclerotic bodies. Mycologic tests are used to confirm the diagnosis. Culture in Sabouraud glucose agar media or Micosel agar allows isolation and identification of causal organisms within about 15 days. The principal causal agent is Fonsecaea pedrosoi, followed by four species in order of frequency, Phialophora verrucosa, Cladosporium carrionii, Fonsecaea compacta, and Rhinocladiella aquaspera [8].
Histologic features of a skin biopsy stained with H&E show a dermal granulomatous infiltrate with a predominance of epithelioid cells surrounding fumagoid bodies.
If not diagnosed and treated early, chromomycosis has a chronic evolutional course. The most frequent complication was secondary bacterial infection. Chronic chromomycosis also has potential association with epidermoid carcinoma (14 cases are reported in the literature) [9]. Central nervous system invasion is possible and may be fatal [10].
Our patient presented with a 1½ years duration tumor. Surgical removal followed by oral terbinafine therapy was associated with a favorable outcome—a complete remission within a 3-year followup period.
Treatment in localized lesions can be surgical as in our patient. Widespread lesions can be treated with itraconazole (100-200 mg/day) monotherapy [11] or its combination with oral 5-fluorocytosine (100-200 mg/day) [12]. In long-standing cases, removal of prominent cutaneous lesions by shave excision plus cryotherapy is also very helpful. Terbinafine (250-500 mg/day) for up to 12 months achieved good results in 42 Malagasy patients suffering from chromoblastomycosis [13]. Amphotericin B (1mg/kg/day) intravenously has been used in severe forms.
Chromomycosis is quite rare in our country; diagnosis was made by the histopathologic identification of fumagoid cells and then cultures revealing Fonsecaea pedrosoi. Even in Maghreb, dermatologists should be aware of this diagnosis. For limited involvement, treatment of choice appears to be excision followed by oral terbinafine.
References
1. Esterre P, Andriantsimahavandy A, Ramarcel ER, pecarrere JL. Forty years of chromoblastomycosis in Madagascar: a review. Am J Trop Med Hyg 1996;55:45-47. PubMed2. Maslin J, Morand JJ, Civatte M. Chromomycoses (chromoblastomycoses). Med Trop 2001;61:459-61. UI 11980389. PubMed
3. Jarmouni R, Ntidam H, Afailal A, Najjam F, Habib Eddine S, Guessous N, Lakhdar H. Les mycoses profondes (A propos de 30 cas). Rappports du XIXè Congrès de l’Association des Dermatologistes et Syphiligaraphes de Langue Française, Rabat, 12-15 mai 1989 : 39-43.
4. Perrin P, Moulonguet I, Chemaly P, Marinho E, Traoré F, Badill et al. Chromomycose chez une patiente algérienne. Journées dermatologiques de Paris, 8-11 mars 1989, Paris, Poster 55.
5. Boughdène-Stambouli C, Belbachir OH, Bariout H. La chromomycose : à propos de 7 cas. Ann Dermatol Venereol 2001 ;128 :S21-S27, C29.
6. H. Marrak, N. Mnajja, S. Fenniche, M. Fourati, M. Zghal, E. Chaker, M. Ben Ayed, I. Mokhtar. Chromomycose: A propos d’une observation. J Mycol Med 2003;13:37-39.
7. Minotto R, Bernardi CD, Mallmann LF, Edelweiss MI, Scroferneker ML. Chromoblastomycosis: a review of 100 cases in the state of Rio Grande do Sul, Brazil. J Am Acad Dermatol 2001;44:585-92. PubMed
8. Bonifaz A, Carrasco-Gerard E, Saul A. Chromoblastomycosis: clinical and mycologic experience. Mycoses 2001;44:1-2. PubMed
9. Esterre P, Pecarrere JL, Raharisolo C, Huerre M. Squamous cell carcinoma arising from chromomycosis. Report of two cases. Ann Pathol 1999;19:516-20. PubMed
10. Artüz F, Alli N, Lenk N, Güngör E. Purple erythematous plaques on the face and left arm. Arch Dermatol 1997; 133:1027-1032. PubMed
11. Smith CH, Barker JN, Hay RJ. A case of chromomycosis responding to treatment with itraconazole. Int J Dermatol 1993;128:436-9. PubMed
12. Bolzinger T, Pradinaud R, Sainte-Marie D, Dupont B, Chwetzoff E. Traitement de quatre cas de chromomycose à Fonsecaea pedrosoi par l’association 5-fuorocytosine-itraconazole. Nouv Dermatol 1991;10 :462-6.
13. Hay RJ. Therapeutic potential of terbinafine in subcutaneous and systemic mycoses. Br J Dermatol. 1999;141 Suppl 56:36-40. PubMed
© 2005 Dermatology Online Journal

