Lichen planus pigmentosus-inversus: Case report and review of an unusual entity
Published Web Location
https://doi.org/10.5070/D356c7h5ntMain Content
Lichen planus pigmentosus-inversus: Case report and review of an unusual entity
Erich Gaertner MD1, William Elstein MD2
Dermatology Online Journal 18 (2): 11
1. SaraPath Diagnostics, Sarasota, Florida2. Cosmetic and Comprehensive Dermatology, Sarasota, Florida
Abstract
Lichen planus pigmentosus-inversus is a rare variant of lichen planus, with less than 20 cases reported in the medical literature. It presents as asymptomatic to mildly pruritic, hyperpigmented macules and/or patches involving intertriginous and flexural areas and skin folds in light-skinned individuals. The unique pattern of skin involvement, clinical features, and histology are distinctive. The combination of hyperpigmented lesion(s) isolated to non-sun exposed, intertriginous, and flexural areas with lichenoid histology is unique and separates it from other similar entities, such as lichen planus actinus and erythema dyschromicum perstans/ashy dermatosis. The case well highlights this unusual condition and represents the first case reported in the United States.
Introduction
Lichen planus pigmentosus-inversus is a rare variant of lichen planus, with less than 20 cases reported in the medical literature. It presents as asymptomatic to mildly pruritic hyperpigmented macules and/or patches involving intertriginous and flexural areas and skin folds, most commonly the axilla and groin, in light-skinned individuals. The majority of reported patients have been white or Asian and are generally without other skin lesions. Nail, scalp, or oral lesions are absent. Histologically the biopsies show a variably dense lichenoid infiltrate of lymphocytes and histiocytes with epidermal atrophy and prominent pigmentary incontinence in the superficial dermis. The lesions show a variable course, with some spontaneously resolving and others remaining for years. The skin lesions are generally resistant to treatment. The unique pattern of skin involvement and clinical features, combined with the histology, are distinctive, and separate it from other similar entities, such as lichen planus actinus and erythema dyschromicum perstans/ashy dermatosis. The case well highlights this unusual entity, and represents the first case reported in the United States.
Case report
A 58-year-old male presented with a several week history of asymptomatic, enlarging, hyperpigmented patches involving the groin and adjacent flexural folds bilaterally. No associated pruritus was present and there were no oral, hair, nail, or other skin lesions. He was in good health, without systemic symptoms or history of malignancy. He denied any recent drug/medication use. On physical examination, the patches were linear in appearance, with long axis following the flexural fold; each measured 5 cm in greatest dimension. They were purple-brown macules and had no associated erythema or scale. No other lesions or skin, nail, or scalp changes were present. Skin scrapings were negative for fungal organisms on potassium hydroxide preparation and all laboratory data, complete blood count, liver function tests, and electrolytes, were within normal limits. Hepatitis C serology was negative.
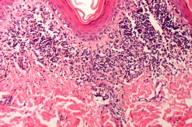
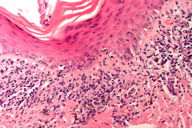
Bilateral skin biopsies showed identical features, both demonstrating dense, band-like interface lymphohistiocytic inflammation with associated basilar vacuolar change and scattered apoptotic keratinocytes. The epidermis was thinned with overlying orthokeratosis. Prominent pigmentary incontinence with numerous melanin-containing macrophages was present in the superficial dermis. Deep inflammation, perifollicular inflammation, eosinophils, or plasma cells were not present. The lymphocytes were unremarkable and lacked atypical architectural or cytologic features. PAS stain was negative for fungal organisms and Alcian blue stain was negative for increased dermal mucin. A103 immunohistochemical stain was negative for an atypical melanocytic process. Based on the pattern of involvement and clinical and pathologic features, the diagnosis of lichen planus pigmentosus-inversus was made. The lack of drug/medication history would exclude fixed drug eruption and the characteristic clinical features and location (light skinned individual in non-sun exposed, flexural areas without other lesions) would exclude lichen planus actinicus and ashy dermatosis.
Discussion
Lichen planus pigmentosus was initially described in India and occurs in darker skinned individuals, most commonly on the face, trunk, and upper extremities, with intertriginous involvement seen infrequently [1]. Lichen planus pigmentosus-inversus was initially described in the Czech Republic in seven white, Eastern European patients and primarily involves intertriginous areas (axilla and groin), with other skin involvement uncommon. Given the lesions showed similar clinical and histologic appearance, manifested by hyperpigmented, brown macules and/or patches, the authors coined the term lichen planus pigmentosus-inversus [2]. Lichen planus pigmentosus-inverus is a rare variant of lichen planus, with fewer than 20 cases reported in the literature [2-10].
Lichen planus pigmentosus-inverus generally occurs in light-skinned individuals in non-sun exposed, intertriginous and flexural areas and skin folds. Whites and Asians have been most commonly reported, with the axilla most consistently involved (over 90% of reported cases) [2-9]. The groin, intramammary area, popliteal fossa, and flexural folds of the neck have also been reported [2]. In a minority of patients, additional lesions with features of lichen planus or lichen planus pigmentosus can be found outside the flexural areas, but these are sparse, accounting for no more than 10 percent of the entire area of involvement [2]. Lesions outside the intertriginous areas are seen in only approximately 10 percent of cases [5]. Association with hepatitis C has been reported, but is uncommon [5]. Two cases of lichen planus pigmentosus-inversus have arisen in association with longstanding lichen planus-inversus [9]. Although a case of paraneoplastic lichen planus pigmentosus was reported, this has not been seen with lichen planus pigmentosis-inversus [11].
The lesions generally present as hyperpigmented, sharply defined brown macules to patches, ranging in size from less than one centimeter to several centimeters. As reported by Pock et al in the initial report, “The larger lesions tend to be a linear or angular configuration. The long axis of the lesion follows the lines of cleavage” [2]. Wickham striae have been rarely reported [2]. Lesions have been present for weeks to up to 15 years. The condition is generally asymptomatic or only slightly pruritic. Mucosal, scalp, and nail involvement is absent. The clinical course is variable, with some cases disappearing within weeks without therapy, whereas others can persist for years. Treatment with tacrolimus, other calcineurin inhibitors, and high potency steroids has had variable, but limited, success in isolated cases. One author notes that at least eight weeks of tacrolimus therapy is required for noticeable results (decrease in pigmentation) [3].
Reported biopsy findings have all been similar, showing an orthokeratotic, atrophic epidermis with variably prominent lichenoid inflammation containing lymphocytes and histiocytes. There is prominent pigmentary incontinence and melanin containing macrophages in the superficial dermis. The rapid onset of an intense lichenoid reaction is theorized to cause the combination of epidermal atrophy and marked pigmentary incontinence without epidermal hyperplasia as is often seen with lichen planus. The melanin deposition is in the superficial dermis as opposed to ashy dermatitis in which it is present deeper in the dermis leading to the bluish-grey color from the Tyndall effect [5].
Lichen planus pigmentosus-inversus is a rare variant of lichen planus, with unique clinical features as described. The combination of hyperpigmented lesion(s) isolated to non-sun exposed, intertriginous and flexural areas with lichenoid histology is unique for this entity. We report the first case described in the U.S. literature and expand the known case material. This unusual entity should be considered in the subset of patients with hyperpigmented intertriginous macules, especially in light-skinned individuals.
References
1. Bhutani LK, Bedi TR, Pandi RK, Nayak NC. Lichen planus pigmentosus. Dermatologica. 1974; 149:43-50. [PubMed]2. Pock L, Jelínková L, Drlík L. Lichen planus pigmentosis inversus. J Eur Acad Dermatol Venereol. 2001;15(5):452-4. [PubMed]
3. Al-Mutairi N, El-Khalawany M. Clinicopathologic characteristics of lichen planus pigmentosus and its response to tacrilomus ointment: an open label, non-randomized, prospective study. J Eur Acad Derm Venereol. 2010;24(5):535-540. [PubMed]
4. Jung YJ, Lee YH. A case of lichen planus pigmentosus-inversus in a Korean patient. Ann Dermatol. 2011:23(1):61-63. [PubMed]
5. Bennassar A, Mas A, Julia M, et al. [Annular plaques in the skin folds: 4 cases of lichen planus pigmentosus-inversus]. Actas Dermosifiliogr. 2009;100(7):602-5. Spanish. [PubMed]
6. Kim BS, Aum JA, Kim HS. Coexistence of classic lichen planus and lichen planus pigmentosus-inversus: resistant to both tacrolimus and clobetasol proprionate ointments. J Eur Acad Dermatol Venereol. 2008;22(1):106-7. [PubMed]
7. Kashima A, Tajiri A, Yamashita A, et al. Two Japanese cases of lichen planus pigmentosus-inverus. Int J Dermatol. 2007;46(7):740-2. [PubMed]
8. Kashima A, Tajiri A, Yamashita A. Pigmented and reticulated plaques of folds: A case of lichen planus pigmentosus-inversus. Eur J Dermatol. 2002;12(3):282. [PubMed]
9. Kim BS, Park KD, Chi SG, et al. Two cases of lichen planus pigmentosus inversus arising from longstanding lichen planus-inversus. Ann Dermatol. 2008;20(4):254-256. [PubMed]
10. Sassolas B, Zagnoli A, Leroy JP. Lichen planus pigmentosus associated with acrokeratosis of Bazex. Clin Exp Dermatol. 1994;19:70-73. [PubMed]
© 2012 Dermatology Online Journal