Hereditary papulotranslucent acrokeratoderma
Published Web Location
https://doi.org/10.5070/D35158q15qMain Content
Hereditary papulotranslucent acrokeratoderma
Carina Rizzo MD, Jennifer Bragg MD, Anthony C Soldano MD, David Cohen MD MPH, Nicholas A Soter MD
Dermatology Online Journal 14 (5): 3
Department of Dermatology, New York UniversityAbstract
A 79-year-old woman presented with a history of peeling of the palms and soles that began in young adulthood, with exacerbation after exposure to water. Her mother, 2 sisters, and a female maternal cousin have similar symptoms. Physical examination showed scale and hyperlinearity of the palms. Brief exposure to water initiated the development of 1 to 2 mm, translucent, white papules that were distributed diffusely on the palmar surface, with a concentration at the palmar margins and pressure points. Histopathologic examination showed an acanthotic epidermis with a central depression that was filled with compact orthokeratosis. The physical examination and histopathologic findings are consistent with a diagnosis of hereditary papulotranslucent acrokeratoderma.
Clinical synopsis
A 79-year-old woman was referred to the Charles C. Harris Skin and Cancer Pavilion Contact Dermatology Section in 2006 for evaluation of peeling of the skin on the palms and soles that began in young adulthood. The patient noted that the skin of the palms became thicker and white several minutes after exposure to water. There was no associated pain, burning, or tingling of the affected skin after water exposure. The accentuated lesions last for approximately one hour after drying. The patient has no history of localized trauma. She denied hyperhidrosis. The patient's mother, two sisters, and a female maternal cousin have a history of similar symptoms. There is no personal or family history of atopy. Neither the patient nor her family members have finely textured scalp hair. A review of systems was unremarkable. Treatment has included topical salicylic acid and lactic acid preparations, occlusive barrier agents (petrolatum), and the use of gloves, all with limited efficacy.
Physical examination
Prior to exposure to water, scale and hyperlinearity with minimal lateral desquamation of the palms was present. Faint, 1-2 mm, skin-colored papules were distributed diffusely on palmar surfaces. The soles were similarly but more subtly affected. Exposure of the left hand to water induced, within minutes, wrinkling of the skin and the accentuation of 1-2 mm, translucent, white papules and plaques that were distributed diffusely on the palmar surface but concentrated at the lateral margins and skin folds.
 |  |
| Figure 1 | Figure 2 |
|---|
Laboratory data
None
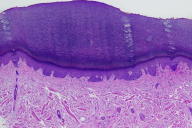
Histopathology
There is mild epidermal acanthosis with a central depression and preserved granular and overlying compact orthokeratosis. The underlying dermis is unremarkable. A van Gieson stain shows normal elastic tissue with in the dermis.
Comment
Hereditary papulotranslucent acrokeratoderma was first described in 1973 [1] as a rare syndrome that is characterized by the onset, at puberty, of asymptomatic, yellow-white, translucent papules and plaques on the palms and soles. Individual lesions are persistent and concentrated at the palmar and plantar margins, pressure points, and areas of trauma. Brief exposure to water initiates rapid wrinkling of palmar and plantar skin. The syndrome appears to exhibit an autosomal-dominant inheritance pattern. The initial cases were associated with finely-textured scalp hair and an atopic diathesis. Skin lesions were characterized histopathologically by focal hyperkeratosis and acanthosis of the epidermis, with normal eccrine ducts and the absence of an inflammatory infiltrate.
The pathogenesis of hereditary papulotranslucent acrokeratoderma remains unknown. Subsequent case reports described a related condition, which was termed transient reactive papulotranslucent acrokeratoderma, aquagenic palmoplantar keratoderma [2], and aquagenic syringeal acrokeratoderma [3]. There were painful translucent white papules that were limited to the palms and that were initiated by brief exposure to water. The lesions completely resolved after drying. Histopathologic examination of lesional skin showed dilated eccrine ostia in a mildly hyperkeratotic stratum corneum [3, 4]. The syndrome also was associated with palmar hyperhidrosis. In contrast to hereditary papulotranslucent acrokeratoderma, the lesions of transient reactive papulotranslucent acrokeratoderma are limited to the palms without any involvement of the soles and resolve completely on drying of the hands. The syndrome was further distinguished by periods of complete remission during which no reaction resulted from water exposure. An autosomal-recessive pattern of inheritance was initially hypothesized [5, 6], but subsequent studies have suggested an acquired process attributed to eccrine dysregulation [3].
Transient reactive papulotranslucent acrokeratoderma has been characterized as a disease primarily affecting young women, although a single affected boy has been described [7]. Two subsequent case reports describe variants of hereditary papulotranslucent acrokeratoderma as it was originally characterized. In 1998, a female patient with persistent, asymptomatic, skin-colored papules diffusely distributed on the palms rather than concentrated at the palmar margins was described [8]. The case was not associated with atopy or fine-textured scalp hair [8]. More recently, a woman with hereditary papulotranslucent acrokeratoderma, which was characterized by persistent, asymptomatic, diffusely-distributed, palmar papules that became acutely pronounced on exposure to water, was reported [9]. This patient demonstrated clinical overlap with transient reactive papulotranslucent acrokeratoderma. Therapeutic interventions for hereditary papulotranslucent acrokeratoderma have been aimed at decreasing hyperkeratosis, such as with topical 12 percent ammonium lactate cream, or providing an occlusive barrier, such as with petrolatum or glycerin, to minimize water exposure [3, 6, 9]. Neither has proved efficacious. Transient reactive papulotranslucent acrokeratoderma has been treated successfully with aluminum chloride hexahydrate. Because this condition is known to spontaneously remit, however, it is unclear that resolution can correctly be attributed to treatment [6]. No cases have been reported of aluminum chloride hexahydrate being used to treat hereditary papulotranslucent acrokeratoderma.
References
1. Onwukwe MF, et al. Hereditary papulotranslucent acrokeratoderma: a new variant of familial punctate keratoderma? Arch Dermatol 1973;108:1082. Yan AC, et al. Aquagenic palmoplantar keratoderma. J Am Acad Dermatol 2001;44:696
3. MacCormack MA, et al. Aquagenic syringeal acrokeratoderma: report of two teenage cases. J Am Acad Dermatol 2001;45:124
4. English JC III, McCollough ML. Transient reactive papulotranslucent acrokeratoderma. J Am Acad Dermatol 1996;34:686
5. English JC III, McCollough ML. Hereditary papulotranslucent acrokeratoderma. Cutis 1998;61:306
6. Itin PH, Lautenschlager S. Aquagenic syringeal acrokeratoderma (transient reactive papulotranslucent acrokeratoderma). Dermatology 2002;204:8
7. Neri I, et al. Transient aquagenic palmar hyperwrinkling: the first instance reported in a young boy. Pediatr Dermatol 2006;23:39
8. Heymann WR. Hereditary papulotranslucent acrokeratoderma. Cutis 1998;61:29
9. Sracic JK, et al. Hereditary papulotranslucent acrokeratoderma: a case report and literature review. Dermatol Online J 2005 1;11:17
© 2008 Dermatology Online Journal

