skin infection: A case report
Published Web Location
https://doi.org/10.5070/D349s9m2t9Main Content
Fusarium skin infection: A case report
Kritika Vishwanath Singhal1 MD, Vikrant Saoji1 MD, Sandhya V Saoji2 MD
Dermatology Online Journal 18 (4): 6
1. Department of Dermatology, Venereology, and Leprosy, Jawaharlal Nehru Medical College, Sawangi, Wardha, India2. Consultant Microbiologist
Abstract
A 65-year-old man presented with an irregular ulcer with a black eschar on his forehead associated with severe headache. A subcutaneous nodule with a necrotic center was present on the left knee. The diagnosis of Fusarium infection was made and confirmed by biopsy and culture. The patient had a history of bronchial asthma for which he was on inhalational steroids for 5 years. It is unclear if this treatment was related to the disseminated Fusarium infection. The patient received oral itraconazole for 3 months with good improvement but met with an unexpected sudden death.
Introduction
Introduction: Fusarium is a filamentous fungus (mold) widely distributed in nature. It rarely infects man. Fusarium causes superficial and localized infection or disseminated infection associated with high mortality [1]. Localized infections are usually seen in immunocompetent hosts and disseminated infections in immunocompromised hosts [1].
Case report
 |  |
| Figure 1 | Figure 2 |
|---|---|
| Figure 1. Ulcer with black eschar on forehead Figure 2. Lesion on left knee | |
A 65-year-old agriculture laborer presented with a skin lesion on his forehead. He had been consulting a physician for severe headaches for 4 months, not associated with nausea or vomiting. The headaches were persistent in spite of painkillers. Fifteen days previously he developed an irregular painful ulcer with a black eschar on his forehead (Figure 1). Erythematous tender nodules with black eschar were seen on the left knee (Figure 2).
Biopsy and diagnosis
 |  |
| Figure 3 | Figure 4 |
|---|---|
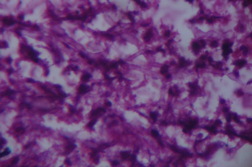
| Figure 3. Fungal filaments in gram stained smear Figure 4. Biopsy showing fungal filaments | |
 |  |
| Figure 5 | Figure 6 |
|---|---|
| Figure 5. Cottony colony of Fusarium Figure 6. Healing of lesion after 2 months | |
 |
| Figure 7 |
|---|
| Figure 7. Healed lesion on left knee |
His leucocyte count was 12,100 with neutrophils (78%), lymphocytes (16%), eosinophiles (4%) and monocytes (2%). Hemoglobin was 10 gm percent. Blood glucose was normal. Liver and kidney function tests were within normal limits. CT scan of the brain was normal. Gram and Zeil-Nelson smears from the lesion were negative. Because of the black eschar the possibility of vasculitis was considered and the patient was started on oral prednisolone 20 mg twice daily. The patient returned on the 3rd day with persisting headache and enlarging of the skin lesion. A skin biopsy was taken. A gram stained smear from the biopsy showed filamentous fungal hyphae (Figure 3). A diagnosis of deep fungal infection was made and aspergillosis was suspected. The patient was started on oral itraconazole, 200 mg twice daily. Within 15 days, headaches subsided and the skin lesions showed signs of healing. The skin biopsy showed hemorrhage, chronic inflammatory infiltrate, and fungal filaments confirming the diagnosis of deep fungal infection (Figure 4). On culture, Fusarium spp. fungus was identified (Figure 5). The exact species of Fusarium could not be identified. Our patient continued itraconazole for 2 months with good improvement (Figures 6 and 7). However, the patient suddenly expired 4 months after diagnosis and the exact cause of death could not be ascertained.
Discussion
Systemic or disseminated infection is usually associated with immunosuppression [2, 3]. Fusarium species in skin can invade blood vessels, resulting in thrombosis and tissue necrosis [4] that causes the formation of a black eschar at the base of the ulcer, as in our case. Hematological dissemination can occur, but it is unclear if both lesions in our case were from primary inoculation in this agricultural worker. Similar angioinvasion with black eschar formation is seen in Aspergillus skin infection. Fusarium infection in an immunocompetent patient presents with localized disease, a chronic course, and usually a good response to treatment [3]. However, disseminated disease usually follows a rapid downhill course with poor response to treatment.
References
1. Nucci M, Anaissie E. Fusarium infections in immunocompromised patients. Clin Microbiol Rev. 2007;20:695-704 [PubMed]2. Gupta AK, Baran R, Summerbell RC. Fusarium infections of the skin. Curr Opin Infect Dis 2000; 13: 121-128. [PubMed]
3. Dignani MC, Anaissie E. Human fusariosis. Clin Microbiol Infect. 2004;10:67-75. [PubMed]
4. Fan Y, Willems L, Leboeuf C, Li W, Lacroix C, Robin M, Socie G, Ribaud P, Verneuil L, Janin A. Skin Microvascular Thrombosis in Fusarium Infection in Two Early Biopsied Cases. Case Rep Dermatol. 2010;2:76-81. [PubMed]
© 2012 Dermatology Online Journal

