Acroangiodermatitis
Published Web Location
https://doi.org/10.5070/D332h5g5k2Main Content
Acroangiodermatitis
Marissa Heller MD, Julie K Karen MD, William Fangman MD
Dermatology Online Journal 13 (1): 2
New York University Department of DermatologyAbstract
A 26-year-old man with a history of chronic primary lymphedema of the left lower extremity presented with elephantiasis, confluent, violaceous, mascerated plaques, and ulcers on the dorsal aspects of the toes of the left foot. Histopathologic examination showed a proliferation of small blood vessels associated with extravasated erythrocytes and hemosiderin deposits consistent with the diagnosis of acroangiodermatitis. Treatment of the focal ulcers includes compression therapy, local wound care, and surgical elimination of the shunt if there is an associated arteriovenous malformation.
Clinical synopsis
A 26-year-old man was referred to the Charles C. Harris Skin and Cancer Pavilion for the evaluation and treatment of ulcers of the toes of the left foot. There was a remote history of a fractured left leg. Chronic primary lymphedema of the left leg developed three years ago. He subsequently developed a deep venous thrombus in his left leg with a pulmonary embolism that required pulmonary endarterectomy. A filter was placed in the interior vena cava, and he was treated with coumadin. Over the past three years, he noted purple skin lesions and development of ulcers on the toes.
Physical examination revealed confluent, violaceous, mascerated plaques with ulcers were present on the dorsal aspects of the toes of the left foot. The dorsal aspect of the foot exhibited verrucous changes. There was 1+ edema of the left foot, and a 1+ dorsalis pedis pulse was noted. The right foot was uninvolved.
 |  |
| Figure 1 | Figure 2 |
|---|
 |
| Figure 3 |
|---|
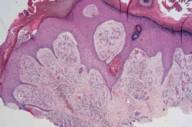
Histopathology reveals a thick papillary dermis with proliferation of capillaries and venules with plump endothelial cells. There are extravasated erythrocytes and hemosiderin deposition. There is an infiltrate of plasma cells and some lymphocytes.
Comment
Acroangiodermatitis, a rare condition that is also known as pseudo-Kaposi sarcoma, is a proliferation of the preexisting vasculature. Clinically, it appears as violaceous or brown macules, patches, papules, or plaques on the distal aspects of the lower extremities. It may be unilateral or bilateral and is commonly located over the extensor surfaces, the lateral malleoli, and the dorsal aspects of the feet. Ulcers may develop over the affected areas [1].
Acroangiodermatitis can be associated with venous hypertension, with an arteriovenous malformation, or with an acquired iatrogenic arteriovenous fistula [1, 2]. A variety of other vascular conditions has been reported in association with acroangiodermatitis. These include limb paralysis, vascular damage from amputation or intravenous drug abuse, the thrombophilic 20210A mutation in the prothrombin gene, and Klippel-Trenaunay syndrome [1, 3, 4, 5].
Histopathologic examination shows proliferation of the capillary bed throughout the dermis. Extravasated erythrocytes, fibrosis with spindle cells, and hemosiderin pigment deposition are noted. There may be a superficial, perivascular infiltrate of lymphocytes, macrophages, and eosinophils. Endothelial cells lining the vessels stain with CD34. A differentiating factor between acroangiodermatitis and Kaposi sarcoma is that in the former, the vascular hyperplasia is of preexisting vasculature and in the latter, the vascular hyperplasia is independent of preexisting vasculature [6].
Treatment of acroangiodermatitis involves correction of the underlying vascular pathology. Mainstays of therapy include compression stockings or a compression pump for venous stasis and local wound care for ulcers. In the case of arteriovenous malformations, surgical correction of the shunt can be employed [7]. Medical therapy options are limited. There is one case report of regression of lesions with treatment with oral dapsone 50 mg twice daily for three months in combination with leg elevation and compression [8]. There are case reports of improvement with oral erythromycin in patients with arteriovenous fistulas for hemodialysis [9].
References
1. Rongioletti F, Rebora A. Cutaneous reactive angiomatoses: patterns and classification of reactive vascular proliferation. J Am Acad Dermatol 2003;49:8872. Samad A, Dodds S. Acroangiodermatitis: review of the literature and report of a case associated with symmetrical foot ulcers. Eur J Vasc Endovasc Surg 2002;24:558
3. Gucluer H, et al. Kaposi-like acroangiodermatitis in an amputee. Br J Dermatol 1999;141:380
4. Martin L, et al. Acroangiodermatitis in a carrier of the thrombophilic 20210A mutation in the prothrombin gene. Br J Dermatol 1999;141:752
5. Lyle WG, Given KS. Acroangiodermatitis (pseudo-Kaposi sarcoma) associated with Klippel-Trenaunay syndrome. Ann Plast Surg 1996;37:654
6. Calonje E, Wilson-Jones E. Vascular tumors: tumors and tumor-like conditions of blood vessels and lymphatics. In: Elder D, et al, eds. Lever's Histopathology of the Skin. 8th ed. Philadelphia: Lippincott-Raven, 1997:914
7. Pires A, et al. Effect of compression therapy on a pseudo-Kaposi sarcoma. Dermatology 1999;198:439
8. Rashkovsky I, et al. Acro-angiodermatitis: review of the literature and report of a case. Acta Derm Venereol (Stockh) 1995;75:475
9. Kim TH, et al. Pseudo-Kaposi's sarcoma associated with acquired arteriovenous fistula. J Dermatol 1997;24:28
© 2007 Dermatology Online Journal

