Retiform purpura in a patient with a history of cocaine use
Published Web Location
https://doi.org/10.5070/D33032v4ncMain Content
Retiform purpura in a patient with a history of cocaine use
A Fthenakis BA1, PA Klein MD2
Dermatology Online Journal 17 (4): 12
1. The George Washington University Medical Center, School of Medicine, Washington, DC2. Department of Dermatology, Stony Brook University Medical Center, Stony Brook, New York
Abstract
There have been rare published cases of retiform purpura related to cocaine use. Levamisole, a common adulterant, has been implicated as the etiologic agent. We describe a female patient, aged 48 years, with cocaine-related retiform purpura involving her face, abdomen, and legs and alert physicians to the dangers of levamisole-contaminated cocaine.
Case report
A 48-year-old woman with a history of cocaine use and no other significant medical problems presented with a three-month history of intermittently appearing purple areas involving her ears, nose, and abdomen, and large tender lesions on her bilateral thighs. She felt well otherwise and denied using any over-the-counter or prescription medications. On repeated further questioning, she admitted to snorting cocaine immediately preceding the eruptions.
 |  |
| Figure 1 | Figure 2 |
|---|
Physical examination revealed stellate-shaped purpuric patches on her abdomen and purpura with erythema on her nose and earlobe (Figure 1 and Figure 2). There was a large, subcutaneous, tender, purpuric plaque on her right thigh. There was no involvement of the palms, soles, or mucous membranes.
A comprehensive laboratory panel included: CBC, Chem 8, LFTs, UA, anti-phospholipid antibodies, anti-cardiolipin antibodies, cryoglobulins, cryofibrinogens, factor V leiden, protein C, protein S, hepatitis C viral antibodies, ANA, Ro, La, C-ANCA and P-ANCA. This work-up revealed only a positive ANA (titer, 1:80) and mildly reduced Protein C and S antigens (63% and 66%, respectively).
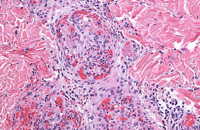 |
| Figure 3 |
|---|
A punch biopsy was obtained from the right thigh for hematoxylin-eosin (H&E) (Figure 3). Histological examination of the biopsy specimen revealed a microvascular thrombosis with vessels containing fibrin thrombi in the superficial and deep vascular plexus and scattered neutrophils. The hematology department was consulted regarding the protein C & S levels and further workup for thrombotic disorders was negative. The diagnosis of levamisole-induced thrombosis with retiform purpura was made based on the histology of the lesions and the history of cocaine use immediately preceding the cutaneous eruptions seen on exam. The patient recovered spontaneously without treatment or scarring. The eruptions appeared again after a subsequent episode of cocaine use.
Discussion
Levamisole, a veterinary anti-helminthic, is a reported contaminant in over 70 percent of the US cocaine supply [1]. This dangerous adulterant has been implicated in several cases of vasculopathy as well as life-threatening agranulocytosis [2, 3]. Reports of retiform purpura related to levamisole are rare but are of increasing importance with higher levels of cocaine contamination. Cutaneous features of levamisole toxity have been described as a retiform purpura with or without skin necrosis. In children who received the drug for nephrotic syndrome, levamisole was implicated in purpuric eruptions of the ears [4].
Histological and immunologic profiles of levamisole toxicity have varied. One case described biopsy specimens revealing a leukocytoclastic vasculitis mixed with thrombosis whereas another revealed only thrombosis without vasculitis [2].
With regard to serologic findings, some cases have noted positive lupus anticoagulant and elevations in antineutrophil cytoplasmic antibodies (ANCAs) directed against proteinase-3 (PR-3) and myeloperoxidase (MPO) [2, 5]. Another case reported small-vessel thrombosis with associated leukocytoclastic vasculitis in a patient with moderately low levels of complement and protein C and S, which is interesting given the depressed levels of protein C & S in our patient [6].
Dermatologists and all physicians should be aware of the potentially life-threatening complication of levamisole in cocaine. Toxicity may mimic a number of conditions including anti-phospholipid syndrome and Wegener granulomatosis [5]. Therefore, it is especially important to pursue a complete history of illegal drug use when forming a diagnosis.
Upon cessation of levamisole, clinical resolution of purpuric lesions occurs within several weeks and serologies normalize within two to fourteen months [2].
References
1. Hitt E. Cocaine laced with levamisole increasing, poses risk for agranulocytosis. Medscape. Accessed September 25, 2010.2. Waller JM, Feramisco JD, Alberta-Wszolek L, et al. Cocaine-associated retiform purpura and neutropenia: is levamisole the culprit? J Am Acad Dermatol. 2010; 63(3):530-535. [PubMed]
3. Zhu NY, Legatt DF, Turner AR. Agranulocytosis after consumption of cocaine adulterated with levamisole. Ann Inter Med 2009; 150:287-288. [PubMed]
4. Rongioletti F, Ghio L, Ginevri F, et al. Purpura of the ears: a distinctive vasculopathy with circulating autoantibodies complicating long-term treatment with levamisole in children. Br J Dermatol 1999; 140: 948. [PubMed]
5. Walsh NMG, Green PJ, Burlingame RW, et al. Cocaine-related retiform purpura: evidence to incriminate the adulterant, levamisole. J Cutan Pathol 2010, no. doi: 10.1111/j.1600-0560.2010.01613.x [PubMed]
6. Bradford M, Rosenberg B, Moreno J, et al. Bilateral necrosis of earlobes and cheeks: another complication of cocaine contaminated with levamisole. Ann Inter Med 2010;152(11):758-759. [PubMed]
© 2011 Dermatology Online Journal

