Digital dermatofibromas - Common lesion, uncommon location: A series of 26 cases and review of the literature
Published Web Location
https://doi.org/10.5070/D32hg6q36kMain Content
Digital dermatofibromas - Common lesion, uncommon location: A series of 26 cases and review of the literature
Larisa M Lehmer MA, Bruce D Ragsdale MD
Dermatology Online Journal 17 (8): 2
Western Dermatopathology, San Luis Obispo, California. llehmer@ccpathology.comAbstract
Dermatofibroma (DF), also referred to as cutaneous fibrous histiocytoma (CFH), is a common tumor of the skin presenting as a firm nodule located predominantly on the limbs and shoulder and pelvic girdles that often extends into superficial subcutaneous tissue. This is a retrospective study of 26 DFs located on digits. All case slides were retrieved from saved files for diagnostic verification. One case was rejected after revision of the diagnosis to giant cell tumor of the tendon sheath. The 26 remaining cases constitute this reported series. Digital DFs affected 27 to 70 year-olds in a 2.25:1 male to female ratio. The most common clinical diagnosis submitted was "growth" or wart. In only 6 out of the 26 cases was the pre-biopsy diagnosis of DF ventured. Although lesional tissue went to dermal margins in 14 specimens, only one has been re-excised in follow up ranging from 2 months to 10 years. Because DFs can resemble several entities including leiomyosarcoma and dermatofibrosarcoma protuberans, a lack of familiarity with the occurrence of DF on the digits may result in more aggressive treatment than otherwise necessary. DF should be in the differential diagnosis of circumscribed, firm nodules presenting on the digits.
Introduction
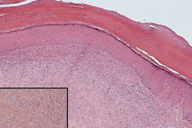
Dermatofibroma (DF) is also referred to as cutaneous fibrous histiocytoma. DFs are solitary, slowly growing nodules that usually appear during early to mid-adult life and can occur in response to minor trauma or insect bites [1]. They are most commonly found on the extremities, shoulder, and buttocks. DFs are relatively common and account for approximately 3 percent of all specimens submitted to dermatopathology [2]. DFs can be protuberant, plaque-like, or umbilicated (Figure 1) with a storiform histopathologic pattern comprised of spindle-shaped and angular collagen synthesizing cells (Figure 2). Although any surface of the skin may be affected, DFs are most common on the lower extremities [3]. Presentation on the digits is uncommon and is not commonly reported in the literature [4, 5, 6]. Of the 26 cases of benign DF on a digit presented in this series, less than 25 percent were accurately predicted on clinical examination. Dermatologists should include digital DF in their differential diagnosis of circumscribed lesions on a digit to ensure proper treatment.
Materials and Methods
Approximately 5,000 DFs were diagnosed at Western Dermatopathology between 2000 and the conclusion of this study; of these 26 arose on a digit (0.5%). Clinical information was obtained from laboratory request forms, in conversation with contributing clinicians, and by follow up letters. Efforts to pinpoint the precise locations were successful in 18 cases (69%) (Figure 4). All tissue was fixed in 10 percent buffered formalin, routinely processed and embedded in paraffin wax. Sections, 4 mm thick, were stained with hematoxylin and eosin. In 9 selected cases, sections from paraffin blocks were subjected to appropriately controlled immunohistochemical reactions employing Melan-A, HMB45, S100 protein, factor XIII, CD31, CD34, actin, and desmin (Table 1).
The biopsy margins were positive in 14 specimens (Table 2). The rarity of clinically concerning recurrence or persistence was established through a clinical database search of patient histories from the time of the DF biopsy to the final draft of this report, searching for a second specimen at the same site, and augmented by calls and follow up letters to physicians.
Results
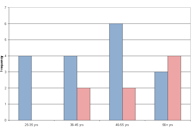
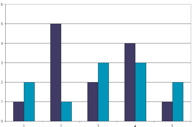
Twenty-six cases of benign DFs of the digit were collected over a ten-year time period from a volume of 225,400 skin specimens (0.01%).* Eighteen males and 8 females (M:F = 2.25:1) between the ages of 27 and 70 years (mean age: 49, median: 52) were affected (Figure 3). Twenty-four cases involved the fingers, whereas only 2 lesions were on the toes. In only 6 cases was the pre-biopsy diagnosis accurate (23%). Most (14, 54%) were sampled by shave biopsy and only one was re-biopsied as a persistent lesion. Only one finger lesion previously partly sampled by shave biopsy was re-excised and this was 9 months after biopsy. We can be confident in the strength of this indicator because the practice from which this study was conducted is in an area with a stable population and the practitioners are loyal to our dermatopathology service.
* An early portion of this series was first introduced as an abstract in the American Journal of Dermatopathology as a 10-patient review. Ragsdale, BD. Digital Dermatofibromas. Am J Dermpathol 2006;28(3):231.
Clinical Findings
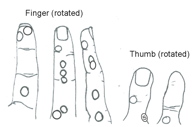
Clinically, lesions presented as firm, well-defined nodules (Figure 1), ranging from 2 to 14-mm in size with a mean diameter of 7.3 mm. Clinical features for all 26 cases are summarized in Table 2. Precise lesion locations were specified for 18 DFs: 17 on fingers and 1 on the left second toe (dorsal aspect) (Figure 4). In the other cases, the location was specified simply as "nth left/right digit." Dorsal (9) and side (6) digital surfaces were similarly disposed to finger DFs whereas the palmar/plantar (4) aspect was less frequently involved (Figure 4). Only four patients had prior, concurrent or subsequent solitary DFs, none of which were also on digits.
Of the 26 digital DFs, 15 were submitted with a clinical impression, only six of which correctly predicted DF. Other clinical diagnoses ventured were mass (4), wart (3), nodule (1), growth (2), lesion (1), neurofibroma (1), and fibroma vs. leiomyoma vs. spiradenoma (1).
 |
| Figure 5 |
|---|
| Figure 5. The left index finger has the highest incidence of DF (n = 24). |
Out of the 24 cases of DFs on fingers, there was a slight predilection for the left side: 13 cases presented on the left hand, 11 on the right. The fingers most frequently affected were the left second and right fourth. Patients with DFs on the left hand tended to have lesions on the 2nd and 3rd fingers, whereas DFs on the right hand were more evenly distributed amongst the digits (Figure 5).
In 5 instances, tumor was at the deep and/or peripheral margins of the specimens. However, only one patient is known to have had a second excision which followed 9 months after the initial biopsy to clear the persistent lesion. Hence, no true "recurrence" (re-growth) has occurred in a follow-up period of up to 10 years.
Histological Findings
No histologic pattern differences were seen between the digital DFs in this series and non-digital DFs (Figure 2). The same fairly well circumscribed dermal expansion of bland angular fibroblasts characterizes these lesions. Only two cases had pattern peculiarities worthy of comment. One featured a central circumscribed superficial tangle of effete capillary channels comprised of thickened tubular basement membranes surrounding a few CD31/factor VIII-positive cells, a pattern that has previously been termed "keloidal" [7]. The other had histologic transition into sclerotic fibroma as reported by Sohn et al (2002) [8].
Immunohistochemical Findings
Eight lesions were tested for factor XIIIa, and all but one were reactive. Three cases were reacted for CD34 and all were negative. All 3 cases analyzed for S100 reactivity were negative, excluding both spindle cell melanocytic lesions and neural differentiation.
Discussion
Also known as cutaneous fibrous histiocytoma (CFH), DFs are one of the most common mesenchymal tumors of the skin. They may occur anywhere on the body [9], but have a predilection for the extremities [10]. Histologically, DFs are unencapsulated, well circumscribed tumors located in the reticular dermis with occasional extension into the superficial subcutis along interlobular septae. DFs are primarily composed of short spindle-shaped and stellate cells, sometimes with a mixture of giant cells, foamy macrophages, siderophages, lymphocytes, and plasma cells [11]. These factor XIIIa positive, benign fibrosing overgrowths of dermal dendrocytes [12] often induce overlying pigmented epidermal hyperplasia [13] and did so on the digits.
Other tumors that present as firm, circumscribed nodules that enter the histopathologic differential diagnosis with DF include perineurioma [14], superficial acral fibromyxoma (SAF), acral dermatofibrosarcoma protuberans (ADFSP), acral fibrokeratoma (AFK), cellular digital fibroma (CDF) [15], sclerotic fibroma, fibroma of tendon sheath, neurofibroma, traumatized wart with dermal fibrosis, and dermal nodular fasciitis. However, clinicopathologic correlation will help distinguish between each of these entities. SAF, for example, arises almost exclusively on the subungual or periungual regions of fingers and toes of middle-aged adults [16] with the big toe as the most frequently affected site [17]. SAFs are composed of spindled and stellate-shaped cells with random, loose storiform, and fascicular growth patterns [17] situated in a myxoid or collagenous stroma, often with accentuated vascularity and increased numbers of mast cells. AFKs are solitary, dome-shaped or elongated thin horns, 1 to 3 mm in diameter and up to 15 mm in height that present predominantly on the fingers [18]. The epidermal covering in an AFK usually shows hyperkeratosis and sometimes acanthosis. AFKs possess a core of thick collagen bundles oriented predominantly along the vertical axis accompanied by stellate fibroblasts. Extraneural (soft tissue) perineuriomas are composed of EMA-positive plump cells with elongated, bipolar cytoplasmic processes [19]; they are relatively uncommon and occur most often on the trunk and extremities of middle aged adults. On low power perineuriomas usually resemble neurofibromas [20], with fascicles or individual cells oriented either parallel to each other or forming small concentric whorls (onion bulbs) - an important clue to the diagnosis [21]. Dermatofibrosarcoma protuberans (DFSP) is a locally aggressive dermal tumor which almost invariably extends into the subcutis with local recurrence in up to 33 percent of cases [22]. It rarely occurs on the digits (acral) in adults [23]. Histologically, DFSP are CD34-positive, factor XIIIa-negative spindle-cell tumors, usually larger than a DF, with a superficial grenz zone and rare deep extension to underlying muscle [24]. CDF is composed of intersecting fascicles of thin, delicate spindle cells in the superficial reticular dermis with a fibrotic and slightly myxoid stroma [25]. CDF is histogenetically distinguished from DF, angiofibromas, and digital fibrokeratomas by strong CD34 staining of its constituent cells with scattered stromal cells expressing factor XIIIa [15]. Sclerotic fibroma has the less cellular "plywood" appearance to its storiform collagen. Fibroma of the tendon sheath has a deeper location the operative note would confirm. Neurofibroma would be S-100 positive. A traumatized wart should have more hypergranulosis and possibly koilocytosis, not present in the epidermal hyperplasia induced by DFs. Dermal nodular fasciitis is diffusely positive for smooth muscle actin but not Factor XIIIa [26]. Rarer keratin-positive considerations would be the keratin and EMA-positive tumors, monophasic synovial sarcoma and fibroblastic variant of epithelioid sarcoma. Acral myxoinflammatory fibroblastic sarcoma should contain bizarre virocyte or ganglion-like giant cells [27]. Low grade fibromyxoid sarcoma with alternating collagenous and myxoid areas has a deceptively bland spindle cell morphology; gene expression profiling shows upregulation of the mucin 4 (muc4) gene, and it has a t(7;16) translocation involving FUS and CREB3L2 [28]. Desmoplastic fibroma is presumed the bony counterpart of soft tissue desmoid-type fibromatosis and would not enter the differential diagnosis except in a vacuum of clinical information.
While there have been many important studies elucidating the clinico-pathologic features of various types of DFs and histiocytomas, presentation of DFs on the digits is very rarely discussed in the literature. A six-case series of DFs on digits conducted by T. Yamamoto et al is significant for its clinical photographic documentation of DFs located on dorsal, medial, and interdigital aspects of the digits [1]. As in that series, the present study found the incidence of DF's on a digit to be higher in males than females in a 2:1 ratio [1] (Figure 3). All three cases of DF analyzed by Gencoglan et al presented in males [29].
The traumatic theory of DF etiology, supported the report by by Gencoglan et al of 3 cases of palmar DFs (2 on the digits) secondary to puncture/mechanical trauma [15], predicts left hand DFs would be more common because tools are more frequently held in the right hand and a work object in the left, which would place the left at more frequent risk of mechanical impact. Yet this series demonstrates only a very slight predilection for the left hand (54%).
The appearance of 5 to 8 DFs in 4 months has been proposed as sufficient to establish a diagnosis of "multiple eruptive DFs" [30]. Only 4 of the 26 patients had more than 2 DFs, suggesting no enhanced tendency to form such lesions associated with the digital location.
Because of a composition of spindle cells resembling fibroblasts and occasionally prominent foam cells, several dermatopathology texts and articles use the biologically imprecise "cutaneous fibrous histiocytoma" as a synonym for DF. However, the concept of "fibrohistiocytic tumors" is flawed. The proliferating spindle cells in these lesions are generally negative for lysozyme and other histiocyte markers. The term "histiocyte" is often used as a crutch by physicians and pathologists in diagnosing unusual tumors. Heddington has vigorously argued that the term "histiocyte" is absolute because it has been applied uncritically to cells of different types and different lineages. Wick, et al, sum up the argument that the nosologic premise of the "fibrohistiocytic" category is "badly flawed," and that there are no reliable and exclusive markers of "fibrohistiocytic" cells. Even those studies finding reactivity with monoclonal antimacrophage antibodies in cutaneous "benign fibrous histiocytomas" admit that the positive cells may be a reactive infiltrate and not the neoplastic component [31].
Histologically, DFs are most often confused with leiomyosarcoma and dermatofibrosarcoma protuberans (DFSP). Leiomyosarcoma differs from DF in its strictly spindle-shaped nuclei, more conspicuous eosinophilic cytoplasm that stains red on Masson trichrome, more uniform fascicular pattern, focal cytologic atypia, and diffuse positivity for desmin and alpha-smooth-muscle actin. DFSP has a tighter storiform pattern, lacks epidermal changes and cytological polymorphism, has discoid nuclei rather than elliptical [8], and scant pale staining poorly defined cytoplasm, extensively involved in the subcutaneous tissue in classic "honey comb" pattern rather than along interlobular fat septa. It shows diffuse positivity for CD34 rather than factor XIIIa [6].
Giant cell tumors (GCT) of the tendon sheath will be encountered in digits much more often than DFs and present as solitary nodular, multiple nodular, and diffuse lesions composed of fibroblastic and fat-accumulating cells. One case initially diagnosed as a DF was determined upon review for this article to be a GCT of the tendon sheath and rejected from this series.
Conclusion
DFs can occur on any finger or even a toe, although it is rarely the preoperative diagnosis (23%). DFs are more commonly found on the dorsal/lateral (47%, 32%) surfaces of the digits but may present on the palmar (21%) surface as well. DF should be included in the differential diagnosis of circumscribed lesions on digits to ensure proper histologic diagnosis and treatment.
References
1. Weiss SW, Goldblum JR. Fibrous Histiocytoma In: Weiss SW, Goldblum JR, editors. Enzinger and Weiss' Soft Tissue Tumors, 5th Edition. Philadelphia (PA): Mosby Elsevier; 2008. p. 1121-32.2. Weedon D. Chapter 34: Tumors and tumor-like proliferations of fibrous and related tissues In: Weedon D, editor. Weedon's Skin Pathology, Third Edition. China: Churchill-Livingston-Elsevier; 2010. p. 827.
3. Gonzalez S, Duarte I. Benign fibrous histiocytoma of the skin: a morphologic study of 290 cases. Pathol Res Pract 1982; 174:379-91. [PubMed]
4. Yamamoto T, Umeda T, Nishioka K. Dermatofibroma of the digit: report of six cases. Dermatol 2003;207(1):79-81. [PubMed]
5. Schwob VS, Santa Cruz DJ Palisading cutaneous fibrous histiocytoma. J Cutan Pathol 1986;13(6):403-408. [PubMed]
6. Kurzen H, Hartschuh W. [Benign cellular fibrous histiocytoma with erosion of the phalanx] Hautarzt 2003 May;54(5):453-456. Epub 2003 Jan 15. German. [PubMed]
7. Kuo TT, Hu S, Chan HL. Keloidal dermatofibroma: report of 10 cases of a new variant. Am J Surgical Pathol 1998 May;22(5):564-8. [PubMed]
8. Sohn I-B, Hwang SM, Lee SH, Choi EH, Ahn SK. Dermatofibroma with sclerotic areas resembling a sclerotic fibroma of the skin. J Cutan Pathol 2002;29(1):44-47. [PubMed]
9. Nickoloff BJ, Griffiths CEM. The spindle-shaped cells in cutaneous kaposi's sarcoma: histologic simulators include factor XIIIa dermal dendrocytes. Am J Pathol. 1989;135(5):793-800. [PubMed]
10. Zaballos P, Llambrich A, Ara M, et al. Dermoscopic findings of haemosiderotic and aneurysmal dermatofibroma: report of six patients. B J Dermatol 2006;154:244-50. [PubMed]
11. Calonje E, Fletcher C. Review article: cutaneous fibrohistiocytic tumors: an update. Adv Anatom Pathol 1994; 1(1): 2-15. [PubMed]
12. Calonje E, Mentzel T, Fletcher C. Cellular benign fibrous histiocytoma: clinicopathologic analysis of 74 cases of a distinctive variant of cutaneous fibrous histiocytoma with frequent recurrence. Am J Surg Pathol 1994; 18(7): 668-676. [PubMed]
13. McCabe J, Blades Z, McGrath E. Practice: What is your call? Canadian Med Assoc J 2008;179(12):1297-1299. [PubMed]
14. Weiss SW, Goldblum JR. Benign Soft Tissue Tumors and Pseudotumors of Uncertain Type In: Weiss SW, Goldblum JR, editors. Enzinger & Weiss's Soft Tissue Tumors, Third Edition. China: Mosby Elsevier; 2008. p. 1080.
15. Fetsch JF, Laskin WB, Miettinen M. Superficial acral fibromyxoma: a clinicopathologic and immunohistochemical analysis of 37 cases of a distinctive soft tissue tumor with a predilection for the fingers and toes. Hum Pathol 2001;32:704-714. [UI:Fetsch JF, Laskin WB, Miettinen M. Superficial acral fibromyxoma: a clinicopathologic and immunohistochemical]
16. Aste N, Pau M, Aste N, Biggio P. Tuberous sclerosis with unusual giant ungual fibromas. J Eur Acad Dermatol Venereol 2003; 17:100-101. [PubMed]
17. Macarenco RS, Ellinger F, Oliveira AM. Perineurioma. A dintinctive and underrecognized peripheral nerve sheath neoplasm. Arch Pathol Lab Med 2007; 131:625-636. [PubMed]
18. Weedon D. Neural and Neuroendocrine Tumors In: Weedon D, editor. Weedon's Skin Pathology, Third Edition. China: Churchill-Livingston-Elsevier; 2010. p. 831.
19. Zelger B. Clue to diagnosis. Dermatopathology: Practical & Conceptual 2000; 6:80-85.
20. Bathelier E, Ly A, Kanitakis J, et al. Subcutaneous dermatofibrosarcoma protuberans masquerading as a cyst. J Eur Acad Dermatol Venereol 2007; 21:1127-1128. [PubMed]
21. Rabinowitz LG, Luchetti ME, Segura AD, Esterly NB. Acrally occurring dermatofibrosarcoma protuberans in children and adults. J Dermatol Surg Oncol 1994; 20: 655. [PubMed]
22. Sauter LS, DeFeo CP. Dermatofibrosarcoma protuberans of the face. Arch Dermatol 1971; 104:671-673. [PubMed]
23. Weedon D. Tumors and tumor-like proliferations of fibrous and related Tissues. In: Weedon D, editor. Weedon's Skin Pathology, Third Edition China: Churchill-Livingston-Elsevier; 2010. p. 809-44.
24. McNiff JM, Subtil A, Cowper SE, et al. Cellular digital fibromas: distinctive CD34-positive lesions that may mimic dermatofibrosarcoma protuberans. J Cutan Pathol 2005; 32:413-418. [PubMed]
25. Smith K, Skelton H. Cutaneous fibrous perineurioma. J Cutan Pathol 1998;25:333. [PubMed]
26. Gencoglan G, Karaarslan IK, Dereli T, Kazandi AC. Dermatofibroma on the palmar surface of the hand. Skinmed 2008 Jan-Feb;7(1):41-3. [PubMed]
27. García-Millán C, et al. [Multiple eruptive dermatofibromas in 2 patients infected with the human immunodeficiency virus]. Actas Dermosifiliogr 2007 Dec;98(10):702-6. [Spanish.] [PubMed]
28. Ragsdale, BD and Murphy, GF. Tumors of the Skin. In: Silverberg SG, editor. Principles and Practice of Surgical Pathology and Cytopathology, Third Edition. Philadelphia (PA): Churchill-Livingstone; 1997. p. 446-449.
29. Gencoglan G, Karaarslan IK, Dereli T, Kazandi AC. Dermatofibroma on the palmar surface of the hand. Skinmed 2008 Jan-Feb;7(1):41-3. [PubMed]
30. García-Millán C, et al. [Multiple eruptive dermatofibromas in 2 patients infected with the human immunodeficiency virus]. Actas Dermosifiliogr 2007 Dec;98(10):702-6. [Spanish.] [PubMed]
31. Ragsdale, BD and Murphy, GF. Tumors of the Skin. In: Silverberg SG, editor. Principles and Practice of Surgical Pathology and Cytopathology, Third Edition. Philadelphia (PA): Churchill-Livingstone; 1997. p. 446-449.
© 2011 Dermatology Online Journal