Localized cutaneous leishmaniasis of the plantar region: A 40-year outcome
Published Web Location
https://doi.org/10.5070/D36g8550p5Main Content
Localized cutaneous leishmaniasis of the plantar region: A 40-year outcome
Eduardo Schenini Diehl1, Somei Ura2, Raul Negrão Fleury2, Hiram Larangeira de Almeida Jr3, Aldina Maria Prado Barral4
Dermatology Online Journal 14 (12): 15
1. Federal University of Rio Grande do Sul, Brazil. edudermatologista@yahoo.com.br2. Lauro de Souza Lima Institute, Brazil
3. Federal and Catholic University of Pelotas, Brazil
4. Oswaldo Cruz Foundation, Brazil
Abstract
We report the case of a 78-year-old male Brazilian farmer, who presented with an extensive ulcer on the right foot that had an erythematous and raised border. This ulcer involved most of the right plantar region and had persisted for more than 40 years. Satellite erythematous papules and tumor-like growths were also seen on the right ankle. Extracutaneous involvement was not found. Light microscopy showed epithelial hyperplasia and diffuse histiocyte infiltration with intense plasmocytosis. Cultures for fungi and Leishmania were negative. The polymerase chain reaction with specific primers for Leishmania was performed using DNA extracted from the lesions; it showed an amplification of 120 pB. The patient had an excellent response after two 20-day cycles of intra-venous N-methylglucamine antimonate (15mg/Kg/day). Leishmaniasis should be highly considered in the differential diagnosis of chronic ulcers in endemic areas.
Case report
 |  |
| Figure 1 | Figure 2 |
|---|---|
| Figure 1. Plantar ulcerations Figure 2. Tumor-like growths with raised borders and central scarring of the ankle | |
A 78-year-old, white male Brazilian farmer presented to our clinic with an extensive ulcer of the right foot. He described that an erythematous papule with central ulceration appeared initially appeared and gradually enlarged over 40 years. Upon physical examination, a shallow ulcer with an erythematous and raised border covered most of the right plantar region (Fig. 1). The ulcer had never healed during the span of 40 years despite the use of several topical medications (topical antibiotics and proteolytic enzymes) and even skin grafts. The patient complained of local pain. Satellite erythematous papules and tumor-like growths with raised borders and central scarring were also seen on the right ankle (Fig. 2). There was no change in skin sensation and there was no lymphadenopathy or mucosal involvement. The otolaryngological examination yielded normal results.
Syphilis serology, blood smear, liver function tests, and electrocardiogram were normal. Radiological examination of the foot ruled out bone involvement. The Montenegro skin test showed a 20 mm papule; the PPD was negative.
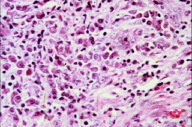
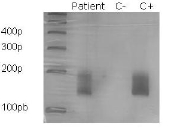
Light microscopy revealed intense epithelial hyperplasia, diffuse histiocyte infiltration with intense plasmocytosis and foci of granulomatous infiltration (Fig. 3). Cultures for fungi and Leishmania were negative. The polymerase chain reaction (PCR) with DNA extracted form the lesions with specific primers for Leishmania showed an amplification of 120 pB (Fig.4).
 |
| Figure 5 |
|---|
| Figure 5. Resolution after the treatment |
The patient had an excellent response after two 20-day cycles of IV N-methylglucamine antimonate (15mg/Kg/day) (Fig.5). After a follow-up of two years there were no recurrences.
Discussion
Localized cutaneous leishmaniasis (LCL) is an infection caused by protozoa of the genus Leishmania and transmitted by sand fly bites [1]. Ninety percent of LCL cases are concentrated in seven countries, including Brazil, where its incidence is apparently increasing [2]. In addition to the classical manifestation [3], numerous atypical forms have already been described, such as acute paronychial, chancriform, annular, palmoplantar [4], zosteriform [4, 5] and erysipeloid [4, 6].
When the infection persists for longer periods the diagnosis is more difficult to establish, because the number of protozoa in the lesions decrease significantly. In these cases, deep fungal and atypical mycobacterial infections must also be considered in the differential diagnosis [3]. In our patient, the prolonged course, the location, and the presence of pain (often absent in LCL) delayed adequate diagnosis for decades.
The Montenegro skin test examines the host's cellular immune response to Leishmania. It consists of an intradermal injection of leishmanial antigen that is read after 48 hours. It is positive if induration exceeds 5 mm. It has a sensitivity of 90 percent, but it has low specificity. In endemic areas, positive results may be obtained in over 50 percent of cases, even in the absence of clinical signs of current or past infection [3, 7]. Nevertheless, an induration of 20 mm is extremely suggestive of active infection.
The culture for LCL carried out using the Novy-MacNeal-Nicolle (NNN) medium has a low sensitivity in chronic cases. Moreover, some Leishmania species grow poorly in this medium and the possibility of bacterial contamination very high [7]. In our case, the culture was negative even in the absence of bacterial contamination.
However, the granulomatous inflammatory infiltrate with intense plasmocytosis found in the biopsy of our patient from an endemic area, combined with a strongly positive Montenegro skin test result, was highly suggestive of LCL [7, 8]. Therefore, we proceded with PCR to confirm the diagnosis.
PCR has gained increasing importance in the diagnosis of LCL. It is more sensitive than conventional histopathological analysis, especially for older lesions [4, 7, 9]. PCR for Leishmania utilizes primers (specific DNA sequences) that amplify a DNA region found in all Leishmania species. The amplification product is shown by gel electrophoresis using 10 percent polyacrylamide [7]. Our patient's excellent response to treatment further confirmed the diagnosis. LCL should always be considered in the differential diagnosis of chronic ulcerations in endemic areas.
References
1. Murray HW, D Berman JD, Davies CR, Saravia NG. Advances in leishmaniasis. Lancet 2005; 366: 1561-1577. [PubMed]2. Desjeux P. Focus: Leishmaniasis. Nature Reviews Microbiology 2004;2:692-693. [PubMed]
3. Salman SM, Rubeiz NG, Kibbi AG. Cutaneous leishmaniasis: clinical features and diagnosis. Clin Dermatol 1999;17:291-296. [PubMed]
4. Raja KM, Khan AA, Hameed A, Rahman SB. Unusual clinical variants of cutaneous leishmaniasis in Pakistan. Br J Dermatol 1998;139:111-113. [PubMed]
5. Omidian M, Mapar MA. Chronic zosteriform cutaneous leishmaniasis. Indian J Dermatol Venereol Leprol 2006;72:41-42. [PubMed]
6. Karincaoglu Y, Esrefoglu M, Ozcan H. Atypical clinical form of cutaneous leishmaniasis: erysipeloid form. Int J Dermatol 2004; 43: 827. [PubMed]
7. Vega-López F. Diagnosis of cutaneous leishmaniasis. Curr Opin Infect Dis 2003;16: 97-101. [PubMed]
8. Mehregan DR, Mehregan AH, Mehregan DA. Histologic diagnosis of cutaneous leishmaniasis. Clin Dermatol 1999; 17: 297-304. [PubMed]
9. Lanus EC, Pinero JE, Gonzales AC, Valladares B, de Grosso ML, Salomon OD. Detection of Leishmania braziliensis in human paraffin-embedded tissues from Tucuman , Argentina by polymerase chain reaction. Mem Inst Oswaldo Cruz 2005; 100:187-192. [PubMed]
© 2008 Dermatology Online Journal