Eruptive neutrophilic xanthomas
Published Web Location
https://doi.org/10.5070/D39zx4v7f1Main Content
Eruptive neutrophilic xanthomas
Bishr Aldabagh MD1, Wilma Bergfeld MD2
Dermatology Online Journal 16 (4): 6
1. Department of Medicine Akron General Medical Center, Akron, Ohio. baldabagh@agmc.org2. Department of Dermatology Cleveland Clinic, Cleveland, Ohio
Abstract
Cutaneous eruptive xanthomas are characteristics lesions of hyperlipidemia. Rarely, these lesions may present with prominent leukocytoclasis as seen in papular neutrophilic xanthomas, which have been described in HIV positive and immunocompromised patients. Herein we describe a patient with eruptive neutrophilic xanthomas with neither hyperlipidemia nor immunocompromise. Moreover, these lesions improved with sun and UV light exposure.
Case report
 |  |
| Figure 1A | Figure 1B |
|---|---|
| Figures 1A and 1B. Shiny indurated papules involving the extremities | |
A 64-year-old Caucasian man with type II diabetes mellitus and polymyalgia rheumatica presented with a two-year history of a skin eruption that progressed to red flat papules, beginning on the trunk and then involving the neck and extremities (Figure 1). The lesions were not painful, but intermittently itchy. Physical exam revealed excoriated, yellow to pink, shiny, indurated papules and small plaques. No lymphadenopathy was present. Colchicine, topical valacyclovir, and a tapering course of prednisone used prior to his presentation had no effect.
Laboratory evaluation revealed WBC 6300 cells/uL, hemoglobin 10.9 g/dL, hematocrit 32.2, MCV 103.8, platelets 248,000/ uL, cholesterol 162 mg/dL, triglycerides 209 mg/dL, HDL 30 mg/dL, LDL 90 mg/dL, VLDL 42 mg/dL, ESR 45, CRP 53 mg/L, LDH 216 U/L, Direct and Indirect Coombs negative, ANA negative, no M-spike on SPEP, PSA of 1 ng/mL, Hep panel negative, and HIV ELISA negative. Blood smear showed no hypersegmented PMNs. Computed tomography scan and colonoscopy were negative for malignancy. The etiology of his anemia remains unclear. Bone marrow biopsy was un-remarkable except for slight hypercellularity. A trial of testosterone did not improve his anemia. He continues to receive transfusions every 2-3 weeks.
 |  |
| Figure 2A | Figure 2B |
|---|---|
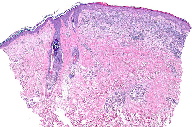
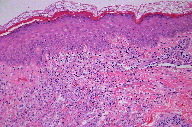
| Figures 2A and 2B. Low power sections reveal a dense inflammatory infiltrate in the papillary and upper dermis (H&E) | |
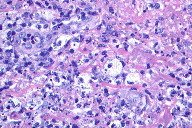
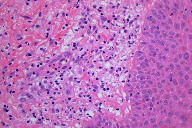
Skin biopsies revealed a superficial xanthomatous infiltrate with a superimposed extensive neutrophilic infiltrate with leukocytoclasia (Figures 2 and 3). Direct immunofluorescence for IgG, A, M, and complement C3 was negative and did not show evidence of leukocytoclastic vasculitis. PAS, GMS, Gram, and Fite stains were also negative. CD117, which is a marker for immature myeloid cells, was negative. Muramidase and myeloperoxidase decorated the numerous neutrophils within the infiltrate. CD30 was negative. PCR for T-cell receptor gamma was also negative.
 |  |
| Figure 3A | Figure 3B |
|---|---|
| Figures 3A and 3B. High power sections reveal numerous xanthoma cells, neutrophils, and neutrophilic debris (H&E) | |
The patient’s dermatitis has never completely cleared; he has periods of near remission and flares. The patient is currently being treated with clobetasol spray, low dose prednisone (for pityriasis rosea), and 3 times per week UV therapy. More recently, he returned from a trip to Phoenix, Arizona, where he received much sun exposure. Now, his rash has significantly improved, and his pruritus is minimal.
Comments
Eruptive xanthomata are characteristic cutaneous lesions of hyperlipidemia, which this patient did not have. Histopathologically, it is unusual for xanthomatous cells to present with very prominent leukocytoclasis. These features may be seen in papular neutrophilic xanthomas, which have been described in HIV-positive patients and those with an underlying lymphoproliferative disease [1, 2]. The patient described here was not HIV-positive and his workup for hematologic and other malignancies was negative. Additionally, his anemia is of unknown cause and did not improve with testosterone supplementation; his bone marrow was neither aplastic nor dysplastic. These facts, coupled with his improvement when exposed to sun and UV light, may point towards an autoimmune etiology.
ACKNOWLEDGMENTS: We would like to thank Dr. Josh Weaver and Dr. Michelle Tarbox for their help with retreiving the images.
References
1. Lima M et al. Atopic dermatitis-like non-erythrodermic leukemic variant of CD3(-/+dim) CD4(+) cutaneous T-cell lymphoma preceded by cutaneous papular xanthomatosis. Leuk Lymphoma. 2004; 45(3): 597-603. [PubMed]2. Smith KJ et. Histologically distinctive papular neutrophilic xanthomas in HIV-1+ patients. Am J Surg Pathol. 1997; 21(5): 545-549. [PubMed]
© 2010 Dermatology Online Journal

