Lupus erythematosus masquerading as erythema multiforme: Does Rowell syndrome really exist?
Published Web Location
https://doi.org/10.5070/D39q89x24rMain Content
Lupus erythematosus masquerading as erythema multiforme: Does Rowell syndrome really exist?
Gunjan M Modi MD1, Angela Shen MD1, Ali Mazloom MD1, Janine Mawad MD2, Aivlys Perez MD3, Michael L Sonabend MD1, Sylvia Hsu MD1
Dermatology Online Journal 15 (2): 5
1. Department of Dermatology, Baylor College of Medicine, Houston, Texas. shsu@bcm.tmc.edu2. Department of Pathology, Baylor College of Medicine, Houston, Texas
3. Department of Dermatology, University of Texas Southwestern Medical Center, Dallas, Texas
Introduction
Rowell syndrome (RS) is a rare entity originally proposed in 1963 by Rowell et al. who described the coexistence of discoid lupus erythematosus with erythema multiforme (EM) in addition to laboratory findings such as positive antinuclear antibody (ANA), rheumatoid factor (RF), and precipitation to a saline extract of human tissue (anti-Sj-T) [1]. Since this syndrome was initially described, a small number of cases of individuals with lupus erythematosus and EM-like lesions have been reported and related to Rowell syndrome. Very few of the reports, however, conformed precisely to Rowell's original stipulations. This article offers a brief review of the evolving diagnostic criteria for RS. In addition, we also present two patients with combined clinical features of lupus erythematosus and EM, initially suggesting RS. However, biopsy of the targetoid EM-like lesions revealed only lupus pathology. Thus, given the lack of histological evidence for erythema multiforme, and lack of a universally accepted set of criteria for diagnosis, this article questions the true existence of Rowell syndrome.
Case reports
Patient 1
 |
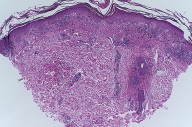
| Figure 3 |
|---|
| Figure 3 Superficial and deep perivascular and periadnexal lymphocytic infiltrates with vacuolar alteration (H&E x40) |
A 28-year-old African-American woman with polycystic ovarian disease was evaluated for a two-week history of well demarcated hypopigmented atrophic patches on her left ear, left cheek (Fig. 1), and bilateral arms, clinically consistent with DLE. There were also scattered erythematous to violaceous targetoid plaques with dusky centers on both palms (Fig. 2) and her left cheek, suggesting concomitant EM. The clinical impression indicated Rowell syndrome given the coexistence of DLE and EM. However, a subsequent 4 mm punch biopsy of the EM-like lesions revealed histological hallmarks of lupus, including basal vacuolar degeneration and a dense superficial and deep perivascular and periadnexal lymphocytic infiltrates (Fig. 3). Further work up showed a 1:320 speckled ANA, negative anti-dsDNA, positive anti-Ro, and negative anti-La antibodies. Due to her proteinuria and hypertension, the patient additionally underwent a renal biopsy, which revealed membranous glomerulonephritis. She was diagnosed with SLE and was treated with hydroxychloroquine, prednisone, and triamcinolone 0.1 percent ointment. Rapid resolution of the targetoid lesions was achieved, but the plaques on her left ear, left cheek, and bilateral arms showed slower resolution with marked postinflammatory leukoderma.
Patient 2
A 44-year-old African-American woman with a long-standing history of systemic lupus erythematosus (SLE) was evaluated for three-month history of progressive scarring alopecia, tan-pink atrophic plaques on both ears, and firm skin-colored papules on both inner canthi and forearms. Given this presentation, her clinical picture was more consistent with discoid lupus erythematosus (DLE). As she was already managed with hydroxychloroquine 200 mg BID and prednisone 10 mg daily by her rheumatologist prior to coming to our clinic, only clobetasol ointment was added, with minimal improvement.
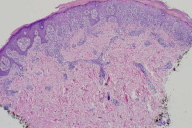
Two years later the patient presented with targetoid dusky plaques on the chest, back, arms (Fig. 4), and dorsal hands. Clinical differential diagnosis at that time included DLE and EM, and the thought of Rowell syndrome was entertained. A biopsy of the targetoid lesions on the right arm showed only findings of lupus erythematosus (Fig. 5), not erythema multiforme. Additional laboratory work-up revealed negative antibodies to double-stranded DNA (dsDNA). The patient was subsequently treated with thalidomide, but was only able to sustain 6 days of therapy due to marked fluid retention. Her prednisone dose was subsequently increased for several weeks with marked improvement.
Discussion
Since the original diagnostic criteria were proposed for Rowell syndrome in 1963, over 40 cases have been reported. None, however, entirely conformed to Rowell's original serologic and clinical standards [2, 3, 4]. In the literature, Rowell syndrome has now been loosely interpreted as any type of cutaneous lupus lesion co-existing with erythema multiforme and associated with various serologies. For example, Dogra et al. [5] reported RS in patients with SLE as opposed to DLE, and Khandpur et al. [6] reported two cases of SLE that were seronegative for anti-Ro and anti-La antibodies. The diagnosis of RS was reported with seronegative antinuclear antibodies by Marzano et al. [7]. In light of this difficulty in respecting Rowell's original criteria, Zeitouni et al. [8] proposed expanding the syndrome to include all cutaneous forms of lupus erythematosus. However, an expansion in the inclusion criteria renders the syndrome both less distinctive and unique.
Also of note is the specificity of the associated laboratory findings for Rowell syndrome. Rowell originally asserted that the serologies in RS, which included positive anti-Sj-antibodies (now thought to be analogous to anti-Ro/ anti-La), speckled ANA, and positive rheumatoid factor (RF), are unique to his syndrome and have not been found in uncomplicated DLE. It is now well known that speckled ANA and anti-Ro/La antibodies are not specific to DLE. Anti-Ro/La antibodies can be found in 20-60 percent of cases of SLE, 70 percent of cases of SCLE, and as well as in Sjogrens, scleroderma, and rheumatoid arthritis [2, 9, 10, 11]. Similarly, the presence of ANA is a non-specific feature, and as many as 35 percent of cases of uncomplicated DLE have a positive ANA, with 5 percent having a titer greater than 1:320 [2, 12]. Among the laboratory criteria of Rowell syndrome, the presence of RF is the probably the least specific. RF is commonly observed in patients with rheumatoid arthritis, Sjogren disease, sarcoidosis, CREST, progressive systemic sclerosis, dermatomyositis, pernicious anemia, and many others conditions [13]. It has even been reported that as many as 5 percent of healthy individuals are positive for RF, increasing to 10-20 percent in people over 65 years old [13]. Thus, the immunological pattern in RS is no longer unique and distinct to justify calling it a syndrome.
While the lack of a consistent and specific serological profile weakens the diagnosis of RS, the very existence of Rowell syndrome is questioned when there is no histological evidence of EM. Rowell syndrome is by definition the coexistence of lupus and EM. Some have suggested that this dual presentation may simply be coincidental associations [4, 8]. The two patients reported here displayed a clinical picture suggestive of Rowell syndrome, but microscopic examination of the targetoid lesions revealed only findings of lupus. From this, one can conclude that the cutaneous presentation of lupus is myriad, with forms including targetoid plaques that mimic EM. Such misinterpretations have been reported by Mendonca [14], in which repeat biopsies of lesions previously read as EM showed lupus instead. It is quite possible that prior reports of RS may be merely lupus masquerading as EM, and that the true existence of Rowell syndrome remains controversial.
References
1. Rowell NR, Beck JS, Anderson JR. Lupus Erythematosus and Erythema Multiforme-Like Lesions. A Syndrome with Characteristic Immunological Abnormalities. Arch Dermatol 1963;88:176-80. [PubMed]2. Shteyngarts AR, Warner MR, Camisa C. Lupus erythematosus associated with erythema multiforme: does Rowell's syndrome exist? J Am Acad Dermatol 1999;40 (5 Pt 1):773-7. [PubMed]
3. Aydogan K, Karadogan S, Balaban Adim S, Tunali S. Lupus erythematosus associated with erythema multiforme: report of two cases and review of the literature. J Eur Acad Dermatol Venereol 2005;19 (5):621-7. [PubMed]
4. Parodi A, Drago EF, Varaldo G, Rebora A. Rowell's syndrome. Report of a case. J Am Acad Dermatol 1989;21 (2 Pt 2):374-7. [PubMed]
5. Dogra A, Minocha Y, Gupta M, Capalash P. Rowell's Syndrome. Indian J Dermatol Venereol Leprol 2000;66 (6):324-5.
6. Khandpur S, Das S, Singh MK. Rowell's syndrome revisited: report of two cases from India. Int J Dermatol 2005;44 (7):545-9. [PubMed]
7. Marzano AV, Berti E, Gasparini G, Caputo R. Lupus erythematosus with antiphospholipid syndrome and erythema multiforme-like lesions. Br J Dermatol 1999;141 (4):720-4. [PubMed]
8. Zeitouni NC, Funaro D, Cloutier RA, Gagne E, Claveau J. Redefining Rowell's syndrome. Br J Dermatol 2000;142 (2):343-6. [PubMed]
9. Cervera R, Khamashta MA, Font J, Sebastiani GD, Gil A, Lavilla P, Domenech I, Aydintug AO, Jedryka-Goral A, de Ramon E, et al. Systemic lupus erythematosus: clinical and immunologic patterns of disease expression in a cohort of 1,000 patients. The European Working Party on Systemic Lupus Erythematosus. Medicine (Baltimore) 1993;72 (2):113-24. [PubMed]
10. Sontheimer RD, Maddison PJ, Reichlin M, Jordon RE, Stastny P, Gilliam JN. Serologic and HLA associations in subacute cutaneous lupus erythematosus, a clinical subset of lupus erythematosus. Ann Intern Med 1982;97 (5):664-71. [PubMed]
11. von Muhlen CA, Tan EM. Autoantibodies in the diagnosis of systemic rheumatic diseases. Semin Arthritis Rheum 1995;24 (5):323-58. [PubMed]
12. Fitzpatrick TB, Freedberg IM. Fitzpatrick's dermatology in general medicine. New York: McGraw-Hill, Medical Pub. Division, 2003.
13. Kasper DL, Harrison TR. Harrison's principles of internal medicine. New York: McGraw-Hill, Medical Pub. Division, 2005.
14. Mendonca R. Lupus erythematosus and erythema multiforme-like lesions. Rowell's syndrome. Dermatol Online J 1997;3 (2):4. [PubMed
© 2009 Dermatology Online Journal