Familial benign chronic pemphigus (Hailey-Hailey disease)
Published Web Location
https://doi.org/10.5070/D39pk6v8zjMain Content
Familial benign chronic pemphigus (Hailey-Hailey disease)
Raegan Hunt MD PhD, Kathryn O’Reilly MD PhD, Jonathan Ralston MD, Hideko Kamino MD, Jerome L Shupack MD
Dermatology Online Journal 16 (11): 14
Department of Dermatology, New York University, New York, New YorkAbstract
We present an atypical case of familial benign chronic pemphigus (Hailey-Hailey disease) that manifested with relapsing, flaccid vesicles and erosions, which were limited to the upper chest, anterior aspect of the neck, and anterior aspects of the upper arms without intertriginous involvement. Although individual eruptions in this patient demonstrated asymmetry, relapses did not obey a segmental distribution. To the best of our knowledge, no other patient has been described with symmetric lesions that were localized solely to the anterior upper body without a prior history of lesions at commonly affected disease sites, which include skin folds, the back, and the posterior and lateral aspects of the neck. This unusual presentation of Hailey-Hailey disease highlights the variable nature of the disease.
History
 |  |
| Figure 1 | Figure 2 |
|---|
A 33-year-old woman presented to the Charles C. Harris Skin and Cancer Pavilion for the evaluation of recurrent, vesicular eruptions that involved her neck, chest, and upper arms. She first noted the lesions in 2005, two months after returning from a hiking trip through the Brazilian Amazon basin. Since then, blisters and crusts of the skin with preceding pruritus and a sensation of burning recur approximately every three-to-four months in the same anatomic distribution. She was unaware of any triggers for her condition and denied any relationship to heat, friction, emotional stress, or menstruation. Similar lesions have never occurred in axillary, inframammary, or inguinal folds or on the oral mucosa. She experienced a single outbreak of genital herpes simplex virus, which was confirmed by a viral culture in 2008. She has been maintained on valacyclovir since that time, with no further genital lesions. Review of systems was unremarkable. Past medical history included migraine headaches. No medications were changed prior to onset of the condition, and the occurrence of new lesions was not influenced by prescription or over-the-counter medications. There were no known blood relatives with a similar condition.
Physical examination
Exudative, eroded, erythematous plaques with crusts were present on the chest, with scattered, pink papules and vesicles. Well-demarcated, irregularly-shaped, pink-brown macules and patches were noted on the anterior aspects of the neck and upper arms. Fingernails were painted, but the patient denied the presence of longitudinal white bands or any other nail abnormalities. There were no mucosal lesions.
Laboratory data
The erythrocyte sedimentation rate was elevated at 63 mm/hr. A complete blood count and comprehensive metabolic panel were normal. Anti-Ro, anti-La, and antinuclear antibodies were negative. Indirect immunofluorescence studies were negative for both intercellular substance antibody (
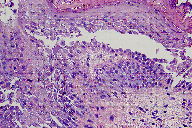
Staphylococcus aureus.Histopathology
There is acantholysis in all levels of the epidermis associated with dyskeratosis and crusting.
Comment
Hailey-Hailey disease, which was first described in 1939 as familial benign chronic pemphigus, is an autosomal dominant acantholytic disorder that manifests with recurrent episodes of painful or pruritic, flaccid vesicles and erosions [1]. Most patients experience initial symptoms during the second or third decade of life and suffer from chronic, relapsing outbreaks. Although any individual’s disease course may be difficult to predict, the majority of patients, who had suffered from the condition for greater than 20 years, felt that their disease became less burdensome with advancing age [2].
The lesions of Hailey-Hailey disease characteristically favor the axillary, genitocrural, and inframammary folds and commonly involve the back and the nape and lateral aspect of the neck [3]. Lesions are typically symmetric although post-zygotic loss of gene function can result in asymmetric type 1 [4] or segmental type 2 [5, 6] disease. Our patient demonstrated an atypical presentation of Hailey-Hailey disease, with symmetrically distributed, recurrent erosions that were limited to the upper chest and anterior aspects of the upper arms and neck. From our literature review, the only other patient reported to have Hailey-Hailey disease lesions that were confined to the anterior upper body without a history of skin fold involvement had experienced many previous lesions on the back and neck, which are favored sites of involvement for Hailey-Hailey disease [7]. Additional unusual presentations of Hailey-Hailey disease include erythroderma [8] and involvement of the vulva, [9] conjunctivae, [10] or mucosae [11, 12]. Asymptomatic longitudinal leukonychia, which was noted in 71 percent of 38 patients with Hailey-Hailey disease, may support the diagnosis in atypical cases [2].
Hailey-Hailey disease results from mutations of the ATP2C1 gene [13]. The rate of sporadic mutations is unclear, partly because of variable expressivity of the disease, but was estimated to be 15 percent in one series of 58 patients [2]. ATP2C1 encodes the protein product hSPCA1, which is a Ca2+/Mn2+ transporter. It is responsible for the local calcium homeostasis in the Golgi apparatus that is required for post translational processing of junctional proteins, which are involved in epidermal cell-cell adhesion [14, 15]. In addition, epidermal cells with mutant hSPCA1 protein demonstrate decreased cellular ATP and abnormal actin remodeling, which are thought to impair formation of adherens junctions [16].
Complications associated with Hailey-Hailey disease include colonization and secondary infections with bacterial, fungal, or viral microorganisms [17], including eczema herpeticum [18], and rare instances of squamous-cell carcinoma [19]. In general, patients experience a relapsing and remitting disease course, with a substantial impact on their quality of life [20]. The frequency of exacerbations may be decreased by wearing light-weight clothing and avoiding activities that result in sweating or skin friction. Topical antimicrobials, oral antimicrobials, topical glucocorticoids, and intralesional glucocorticoids are routinely used to control symptoms [2].
No well-studied or targeted systemic therapy for Hailey-Hailey disease exists although case reports describe the use of cyclosporin, [21] acitretin, [22] and methotrexate [23]. Surgical management with wide local excision of affected skin folds has a high complication rate. Superficial ablative techniques, which include dermabrasion [24] and CO2 or erbium-YAG laser vaporization, [25, 26] and 5-aminolevulinic acid photodynamic therapy [27] have been used with success. Refractory Hailey-Hailey disease may benefit from local electron-beam therapy [28].
References
1. Hailey H, Hailey H. Familial benign chronic pemphigus. Arch Dermatol 1939; 39: 6792. Burge SM. Hailey-Hailey disease: the clinical features, response to treatment and prognosis. Br J Dermatol 1992; 126: 275 [PubMed]
3. Lyles TW, et al. Atypical features in familial benign chronic pemphigus. Arch Dermatol 1958; 78: 446 [PubMed]
4. Hwang LY, et al. Type 1 segmental manifestation of Hailey-Hailey disease. J Am Acad Dermatol 2003; 49: 712 [PubMed]
5. Poblete-Gutierrez P, et al. Allelic loss underlies type 2 segmental Hailey-Hailey disease, providing molecular confirmation of a novel genetic concept. J Clin Invest 2004; 114: 1467 [PubMed]
6. Bittar M ,Happle R. 'Atypical' cases of hailey-hailey disease may represent typical examples of a type 2 segmental manifestation. Dermatology 2005; 210: 182 [PubMed]
7. Saied NK, et al. Atypical familial benign chronic pemphigus. Cutis 1981; 27: 666 [PubMed]
8. Marsch WC , Stuttgen G. Generalized Hailey-Hailey disease. Br J Dermatol 1978; 99: 553 [PubMed]
9. Wieselthier JS , Pincus SH. Hailey-Hailey disease of the vulva. Arch Dermatol 1993; 129: 1344 [PubMed]
10. Oguz O, et al. Conjunctival involvement in familial chronic benign pemphigus q (Hailey-Hailey disease). Int J Dermatol 1997; 36: 282 [PubMed]
11. Vaclavinkova V, Neumann E. Vaginal involvement in familial benign chronic pemphigus (Morbus Hailey-Hailey). Acta Derm Venereol 1982; 62: 80 [PubMed]
12. Fischer H, Nikolowski W. Die Mundschleimhaut beim Pemphigus benignus familiaris chronicus. Arch Klin Exp Dermatol 1962; 214: 261
13. Hu Z, et al. Mutations in ATP2C1, encoding a calcium pump, cause Hailey-Hailey disease. Nat Genet 2000; 24: 61 [PubMed]
14. Durr G, et al. The medial-Golgi ion pump Pmr1 supplies the yeast secretory pathway with Ca2+ and Mn2+ required for glycosylation, sorting, and endoplasmic reticulum-associated protein degradation. Mol Biol Cell 1998; 9: 1149 [PubMed]
15. Hakuno M, et al. Dissociation of intra- and extracellular domains of desmosomal cadherins and E-cadherin in Hailey-Hailey disease and Darier's disease. Br J Dermatol 2000; 142: 702 [PubMed]
16. Aronchik I, et al. Actin reorganization is abnormal and cellular ATP is decreased in Hailey-Hailey keratinocytes. J Invest Dermatol 2003; 121: 681 [PubMed]
17. Zaim MT , Bickers DR. Herpes simplex associated with Hailey-Hailey disease. J Am Acad Dermatol 1987; 17: 701 [PubMed]
18. Stallmann D, Schmoeckel C. Morbus Hailey-Hailey mit Dissemination und Eczema herpeticatum unter Etretinattherapie. Hautarzt 1988; 39: 454
19. Holst VA, et al. Squamous cell carcinoma arising in Hailey-Hailey disease. J Am Acad Dermatol 2000; 43: 368 [PubMed]
20. Gisondi P, et al. Severe impairment of quality of life in Hailey-Hailey disease. Acta Derm Venereol 2005; 85: 132 [PubMed]
21. Berth-Jones J, et al. Benign familial chronic pemphigus (Hailey-Hailey disease) responds to cyclosporin. Clin Exp Dermatol 1995; 20: 70 [PubMed]
22. Berger EM, et al. Successful treatment of Hailey-Hailey disease with acitretin. J Drugs Dermatol 2007; 6: 734 [PubMed]
23. Vilarinho C, et al. Methotrexate for refractory Hailey-Hailey disease. J Eur Acad Dermatol Venereol 2010; 24: 106 [PubMed]
24. Hamm H, et al. Hailey-Hailey disease: eradication by dermabrasion. Arch Dermatol 1994; 130: 1143 [PubMed]
25. Don PC, et al. Carbon dioxide laserabrasion: a new approach to management of familial benign chronic pemphigus (Hailey-Hailey disease). J Derm Surg Oncol 1987; 13: 1187 [PubMed]
26. Beier C, Kaufmann R. Efficacy of erbium:YAG laser ablation in Darier disease and Hailey-Hailey disease. Arch Dermatol 1999; 135: 423 [PubMed]
27. Ruiz-Rodriguez R, et al. Photodynamic therapy with 5-aminolevulinic acid for recalcitrant familial benign pemphigus (Hailey-Hailey disease). J Am Acad Dermatol 2002; 47: 740 [PubMed]
28. Narbutt J, et al. Effective treatment of recalcitrant Hailey-Hailey disease with electron beam radiotherapy. J Eur Acad Dermatol Venereol 2007; 21: 567 [PubMed]
© 2010 Dermatology Online Journal

