Linear psoriasis
Published Web Location
https://doi.org/10.5070/D39kx6x211Main Content
Linear psoriasis
Peter Chien Jr MD PhD, Karla Rosenman MD, Wang Cheung MD, Nadia Wang MD, Miguel Sanchez MD
Dermatology Online Journal 15 (8): 4
Department of Dermatology, New York UniversityAbstract
A 33-year-old man presented with verrucous, red-brown papules, which coalesced into linear plaques on the right buttock, waist, thigh, and genitals. A skin biopsy was consistent with psoriasis, and the unilateral distribution in a linear pattern led to a diagnosis of linear psoriasis, which is a rare variant of psoriasis. Although histopathologically it can be difficult to distinguish from inflammatory linear verrucous epidermal nevus (ILVEN), linear psoriasis presents in adulthood and responds to conventional topical antipsoriatic therapies.
 |  |
| Figure 1 | Figure 2 |
|---|---|
History
A 33-year-old man initially presented to the Dermatology Clinic at Bellevue Hospital Center in February, 2007, with papules on the right buttock, hip, and waist that extended to the groin. Previously administered topical treatments led to clearance of lesions, but the eruption recurred after discontinuation of these agents, the names of which he did not recall. The patient believes that the lesions resulted from unsanitary conditions during imprisonment in Guinea. He currently resides in the United States under political asylum as a torture victim. At the initial visit, the patient was treated with mometasone ointment twice daily to the buttock, hip, and waist and with tacrolimus ointment twice daily to the genitals. A shave biopsy was subsequently performed three weeks later. Subsequent treatments have included tretinoin 0.001 percent gel nightly for two-and-one-half months, triamcinolone 0.1 percent cream twice daily for four months, tretinoin 0.05 percent cream nightly for one month, and fluocinolone 0.01 percent ointment twice daily for one month. With this treatment regimen, the prutitus decreased but the lesions persisted. Clobetasol 0.05 percent ointment applied twice to three times daily for one month resulted in greater improvement in the pruritus. An attempt to prevent adverse effects from class I topical glucocorticoids by changing to triamcinolone ointment for two months resulted in worsening pruritus. Treatment with intralesional triamcinolone acetonide and with topical clobetasol ointment resulted in thinning of the plaques and scattered hypopigmentation. Calcipotriene 0.005 percent cream and triamcinolone ointment applied twice daily produced further improvement. Subsequent use of calcipotriene cream and clobetasol ointment applied twice daily produced further resolution of itching and clearance of many lesions within two months. After he discontinued the topical agents, the lesions began to recur within two weeks.
Past dermatologic history includes verruca vulgaris in the suprapubic area that cleared with trichloroacetic acid 90 percent. Hepatitis B virus infection was diagnosed in June, 2007, but he does not take medications and has no allergies to medications.
Physical Examination
Verrucous, red-brown papules coalescent into linear plaques with depigmented patches were present on right buttock, waist, thigh, and genitals.
Laboratory data
Hepatitis B virus surface antigen without antibody, hepatitis Be antibody, and hepatitis B virus PCR 7.03 x 10² IU/ml were present. Hepatic function panel, basic metabolic panel, and lipid panel are normal. Alpha-fetoprotein was elevated at 12.7 ng/ml. An abdominal ultrasound obtained in September 2007, and a chest radiograph obtained in June 2007, were normal.
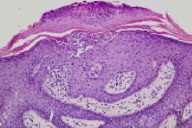
Histopathology
There is a superficial, perivascular and interstitial infiltrate that is comprised of lymphocytes and neutrophils. There is regular epidermal acanthosis, with maintenance of the granular layer and compact orthokeratosis. Focally, there is confluent parakeratosis with hypogranulosis and collections of neutrophils in the stratum corneum and in the spinous layer.
Comment
Linear psoriasis is an exceedingly rare variant of psoriasis. Only a handful of cases have been reported in the literature [1, 2, 3, 4]. Histopathologically it resembles an inflammatory linear verrucous epidermal nevus (ILVEN), and there is some debate as to whether linear psoriasis truly exists as a distinct clinical entity [5]. However, Saraswat et al. described differences in clinical features between the two entities [6]. Inflammatory linear verrucous epidermal nevus tends to develop during the first months of life, progresses slowly, can be very pruritic, and is relatively unresponsive to treatment whereas psoriasis tends to develop later in life, progresses rapidly, is occasionally pruritic, and responds well to antipsoriatic treatment. Immunohistopathologic studies have attempted to further distinguish the two entities. There is lower expression of keratin 10 in psoriasis as compared to normal levels in ILVEN [7, 8]. Inflammatory linear verrucous epidermal nevus lesions without any psoriasis showed lower levels of cell surface expression markers of T-cell subsets, such as CD8, CD45RO, CD2, CD94, and CD161 [8].
Because linear psoriasis develops in the lines of Blaschko, somatic recombination is thought to occur; a gene predisposing to psoriasis in involved, which leads to segmental mosaicism [9, 10]. Other genes acting in concert and environmental factors may then trigger linear psoriasis. One study of two Brazilian children with linear psoriasis showed different associated HLA alleles from those found in other types of early-onset psoriasis [11], although another study found an overlap in allelic association [2]. Despite the unusual morphology of linear psoriasis and its resemblance to ILVEN, linear psoriasis is relatively responsive to antipsoriatic therapies, such as topical dithranol and systemic tumor necrosis factor-a blockade [3, 12]. Because ILVEN is relatively refractory to therapy and often requires surgical or ablative intervention, it may be prudent to pursue a trial of antipsoriatic therapy on the chance that the lesion may be psoriasis.
References
1. Purohit S, et al. Linear psoriasis. Indian J Dermatol Venereol Leprol 2006; 72: 398 [PubMed]2. al-Fouzan AS, et al. Congenital linear psoriasis: a case report. Pediatr Dermatol 1990; 7: 303 [PubMed]
3. de Mare S, et al. Dithranol in the treatment of inflammatory linear verrucous epidermal nevus. Acta Derm Venereol 1989; 69: 77 [PubMed]
4. Rym B, et al. Le psoriasis lineaire de l'enfant. Tunis Med 2005; 83: 429 [PubMed]
5. Goujon C, et al. Le psoriasis lineaire existe-t-il? Ann Dermatol Venereol 1981; 108: 643 [PubMed]
6. Saraswat A, et al. Unilateral linear psoriasis with palmoplantar, nail, and scalp involvement. Pediatr Dermatol 2004; 21: 70 [PubMed]
7. de Jong E, et al. Inflammatory linear verrucous epidermal naevus (ILVEN) versus linear psoriasis: clinical, histological and immunohistochemical study. Acta Derm Venereol 1991; 71: 343 [PubMed]
8. Vissers WH, et al., Immunohistochemical differentiation between inflammatory linear verrucous epidermal nevus (ILVEN) and psoriasis. Eur J Dermatol 2004; 14: 216 [PubMed]
9. Happle R. Somatic recombination may explain linear psoriasis. J Med Genet 1991; 28: 337 [PubMed]
10. Hofer T. Does inflammatory linear verrucous epidermal nevus represent a segmental type 1/type 2 mosaic of psoriasis? Dermatology 2006; 212: 103 [PubMed]
11. Magalhaes RF, et al. Linear psoriasis in Brazilian children and HLA haplotypes. J Eur Acad Dermatol Venereol 2007; 21: 1439 [PubMed]
12. Rott S R, et al. Successful treatment of severe psoriatic arthritis with infliximab in an 11-year-old child suffering from linear psoriasis along lines of Blaschko. Br J Dermatol 2007; 157: 191 [PubMed]
© 2009 Dermatology Online Journal

