Bilateral cutaneous leishmaniasis of upper eyelids: A case report
Published Web Location
https://doi.org/10.5070/D39kq7k2xnMain Content
Bilateral cutaneous leishmaniasis of upper eyelids: A case report
Alireza K Jafari MD1, Maryam Akhyani MD2, Mahin Valikhani MD2, Zahra S Ghodsi MD2, Behrooz Barikbin MD2, and Siavash Toosi MD2
Dermatology Online Journal 12 (1): 20
1. Department of Ophthalmology, Farabi Hospital, Tehran University of Medical Sciences.2. Department of Dermatology, Razi Hospital, Tehran University of Medical Sciences. stoosi@razi.tums.ac.ir
Abstract
An 11-year-old girl presented with a 6-month history of bilateral upper eyelid erythema, induration, and blepharitis resistant to conventional antibiotic therapy. The lesions gradually progressed to symmetrical ulcerative nodules within 3 months. Cutaneous smear and biopsy revealed numerous amastigotes in macrophage cells. Therapy with systemic pentavalent antimonial resulted in successful healing of lesions. We conclude that cutaneous leishmaniasis must be kept in mind in the differential diagnosis of bilateral chronic eyelid swelling in endemic regions of the world.
Introduction
Leishmaniasis is a protozoal disease with diverse clinical manifestations dependent both on the infecting species of the parasite and the immune response of the host. Transmission of the disease occurs by the bite of a sand fly infected with leishmania parasites [1]. It is estimated that 350 million people are at risk of leishmaniasis [2]. Approximately 12 million are affected and 1.5 to 2 million infected each year [3].
The eyelid is involved in only 2.5 percent of cases of cutaneous leishmaniasis, probably because of the movement of the lids that prevents the fly vector from biting the skin in this region [4]. Cutaneous leishmaniasis of the lid may also occur in mucocutaneous leishmaniasis due to L. braziliensis, the infected material reaching the lid from nasal mucosal lesion through the nasolacrimal duct [5].
Clinical synopsis
An 11-year-old girl presented with a 6 month history of bilateral upper eyelid erythema, induration, and blepharitis resistant to treatment with antibiotic eye drops and ointments. The lesions gradually progressed to symmetrical ulcerative nodules within 3 months. Clinical examination revealed two symptomless ulcerative nodules, each one with a nearly 2-cm diameter infiltrated base. These lesions had raised erythematous borders and were located on both upper eyelids. There was considerable edema of the superior eyelids.
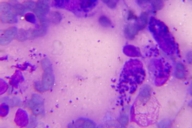
Visual acuity was 20/20 in both eyes. There was no corneal involvement and the ocular examination was normal. Multiple smears from the sore stained with Giemsa were positive for Leishman bodies (amastigotes).
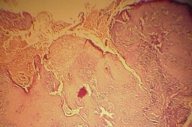
Histopathological analysis showed a heavy mononuclear cell infiltrate with numerous macrophages and granuloma formation with no visible parasites.
Therapy with systemic pentavalent antimonial, 20mg per kilogram of body weight per day, for 3 weeks, resulted in complete healing of the lesions. The patient was entirely normal at a 1 year follow up.
Discussion
Cutaneous leishmaniasis of the eyelid is uncommon in the world. The disease may present diagnostic difficulties when appearing in nonendemic areas. Conjunctiva and sclera are rarely involved and conjunctivitis is generally secondary to contiguous spread from the skin of eyelid or associated with inoculation by the patient's own fingers [4, 6].
Ocular leishmaniasis, particularly its early papulonodular lesions, may simulate other more common conditions such as recurrent chalazion, dacryocystitis, and skin tumors [6, 7, 8, 9]. Nodular, tumor-like lesions, when ulcerated, may resemble keratoacanthomas or basal cell carcinomas, especially in older individuals [10].
In endemic areas the clinical diagnosis is not difficult. Usually, this is best achieved by performing a smear of the material from the sore and staining it with Wright or Giemsa on a microscope slide. Ideally, material should also be cultured on NNN or similar medium. If a biopsy is taken for histological examination, a portion of it should be cultured [11].
In most immunocompetent individuals, the infection and its cutaneous manifestations resolve spontaneously. Treatment with pentavalent antimonial or sodium stibogluconate (pentostam) is typically curative. The more effective treatment is with pentavalent antimonial compounds, and the dosage recommended by the World Health Organization is 20mg/kg per day over 3 weeks [12].
If eyelid lesions remain untreated, contiguous spread may extend to the conjunctiva, episclera, and cornea, with development of interstitial keratitis. Residual scarring and deformity may require surgical correction [13]. Therefore, ocular leishmaniasis is considered potentially a blinding disorder. Physicians working in endemic areas must keep in mind that a high level of suspicion to the diagnosis of cutaneous leishmaniasis and its rigorous treatment is required in order to prevent complications of this potentially blinding disorder.
Reviewing the English literature, we found only one report of a patient with bilateral eyelid lesions caused by cutaneous leishmaniasis that was accompanied by extensive facial involvement [13]. To our knowledge, we report the first case of bilateral and symmetrical cutaneous leishmaniasis that was localized exclusively on both eyelids.
Competing interests: The authors declare that they have no competing interests.
Authors' contributions: All authors contributed equally in the study design, literature search, and data analysis and manuscript
preparation. All authors read and approved the final manuscript.
References
1. Bryceson ADM. Clinical variations associated with various taxa of Leishmania. in; Coll Int CNR/INSERM 1984 Montpelier: IMEEE, 1986:221-8.2. Modabber F. Leishmaniasis. TDR/WHO Rep. 1991-1992. 1993; 8: 77-87.
3. Leishmaniasis. In: Tropical Disease research. WHO Rep. 1993-1994. 1995; 12: 135-46.
4. Abboud IA, Ragab HAA, Hanna LS. Experimental ocular leishmaniasis. Br J Ophthalmol 1970; 54: 256-62.
5. Morgan G. Case of cutaneous leishmaniasis of the lid. Br J Ophthalmol 1965; 49(10):542-6
6. Roizenblatt J. Interstitial keratitis caused by American (mucocutaneous) leishmaniasis. Am J Ophthalmol 1979; 87: 175-9.
7. Abdel-hameed AA, Hassan MEA, Abdalla KM, El-Basha A, Ahmed BO, Mohammadani AA. Two cases of ocular leishmaniasis. Topical and Geographical Medicine 1990: 91-3.
8. O'Neill DP, Deutsch J, Carmichael AJ, Taylor R. Eyelid leishmaniasis in a patient with neurogenic ptosis. Br J Ophthalmol 1991; 75: 506-7.
9. Nandy A, Addy M, Chowdhury AB. Leishmaniasis blepharo-conjunctivitis. Trop Geogr Med 1991; 43: 303-6.
10. Oliveira-Neto MP, Martin VJ, Mattos MS, et al. South American cutaneous leishmaniasis of the eyelids: report of five cases in Rio de Janeiro state, Brazil. Ophthalmology 2000; 107(1):169-72
11. Griffiths WA, Dutz W. Repeated tissue sampling with a dental broach. A trial in cutaneous leishmaniasis. Br J Dermatol 1975; 93:43-5
12. Oliveira-Neto MP, Martins VJ, Mattos MS, Pirmez C, Brahin LR, Benchimol E. South American cutaneous Leishmaniasis of the eyelids: Report of five cases in Rio de Janeiro State, Brazil. Ophthalmology. Volume 107, Issue 1 , January 2000, Pages 169-172
13. Chaudhry IA, Hylton C, DesMarchais B Bilateral ptosis and lower eyelid ectropion secondary to cutaneous leishmaniasis. Arch Ophthalmol. 1998 Sep;116(9):1244-5.
© 2006 Dermatology Online Journal