Myxoid neurothekeoma: A painful case in a less common location
Published Web Location
https://doi.org/10.5070/D39j85n7ncMain Content
Myxoid neurothekeoma - a painful case in a less common location
Uwe Wollina1, Gesina Hansel1, Jaqueline Schönlebe2, Gunther Haroske2
Dermatology Online Journal 15 (4): 3
1. Department of Dermatology and Allergology2. Institute of Pathology "Georg Schmorl"
Hospital Dresden-Friedrichstadt, Academic Teaching Hospital of the Technical University of Dresden, Dresden, Germany. wollina-uw@khdf.de
Abstract
Myxoid neurothekeoma is a rare benign asymptomatic tumor of the skin. Most tumors are located on the head, shoulders and arms. We present a 19-year-old female patient with a relapsing tumor of this type in a less common localization, i.e., lower trunk, and with painful sensations under mechanical pressure. Wide excision surgery led to complete remission.
Introduction
Neurothekeoma is a rare tumor found mostly on the face or limbs of younger patients [1]. There are currently three subtypes of neurothekeoma recognized, based on cellularity of the tumor, growth pattern, and stromal mucin: (a) the myxoid type with hypocellularity, distinctly lobulated growth pattern and abundant myxoid stroma, (b) the cellular type with a fascicular growth pattern, high cellularity and scant mucin and (c) the mixed type that shares features of both (a) and (b) [2, 3].
We present a case with less common localization of a myxoid neurothekeoma in a young female patient.
Case report
 |
| Figure 1 |
|---|
| Fig 1: Clinical presentation of myxoid neurothekeoma. The scar resulted form an incomplete resection 3 years ago. |
A 19-year-old woman presented with a painful subcutaneous nodule on the right lower back that had relapsed within 4 weeks after surgical excision elsewhere three years ago. We found a soft nodular subcutaneous tumor (2.0 x 2.5 cm) (Fig. 1).
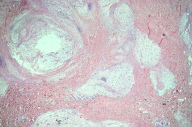
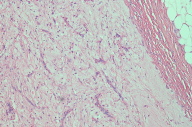
The tumor was removed surgically with wide margins under local anaesthesia. Histopathology demonstrated a nodular, lobulated hypocellular tumor of the dermal and subcutaneous tissue layers. It was composed of plump spindle cell proliferations with a tendency to whorled growth with pronounced myxoid stroma and multiple small vessels (Figs. 2a, 2b). The cells showed abundant and pale cytoplasm and indistinct cellular borders. Mucin deposits were easily demonstrated with Alcian blue staining (Fig. 2c). Tumor cells expressed focally smooth muscle actin (SMA). S-100 protein expression was weak but evident throughout the tumor (Fig. 2d).
 |  |
| Figure 2c | Figure 2d |
|---|
Wound healing was uncomplicated and follow-up did not show a recurrence.
Discussion
Neurothekeoma shows a clear female predominance. More than 75 percent of tumors occur on head, neck, shoulder girdle and arms [4]. Neurothekeoma is traditionally classified as a rare benign neoplasm of putative neural origin [1] but recently there has been disagreement about the differentiation of the cellular type of neurothekeoma [2, 3, 4, 5, 6].
Tumor cells of myxoid neurothekeoma are reactive for vimentin, NKI-C3, CD10, PGP9.5, microphthalmia transcription factor (MiTF), and smooth muscle actin (SMA), but negative for melan-A and glial fibrillary acid protein [4, 5, 6, 7]. CD68 expression may be seen focally in histiocytic areas or in cellular neurothekeoma with histiocytic differentiation [8]. There is some confusion in the literature about S-100 expression. In an analysis of 178 neurothekeomas including myxoid type none of the tumors expressed S-100 [4]. In another study with 22 tumors the authors found that 11 of 11 myxoid neurothekeomas expressed S-100 [7]. It seems that myxoid neurothekeoma can lose the strong S-100B expression when cells are less differentiated. On the other hand S-100A6 has been recommended as a highly sensitive diagnostic marker in immunohistology even for the cellular type that is usually S-100 negative [8, 9].
Differential diagnoses include fibroma, dermatofibroma, leiomyoma, neurilemmoma, neurofibroma, and low-grade sarcoma among others [10, 11].
The presented case shows a less common location for this rare benign tumor of putative neural origin. Pain is an unusual clinical symptom [1, 4]. We assume, that the scar of the first incomplete resection of the tumor might be responsible, not the tumor itself.
Although the majority of neurothekeomas are dermal tumors involvement of subcutaneous tissue is quite common. Regrowth or local recurrences are seen in about 7 percent of patients [4, 10]. Therefore, we concur with those who recommend surgical excision with a wider margin if possible. For the head and neck region micrographic controlled surgery is particularly useful [3, 12, 13].
References
1. Gallager RL, Helwig EB. Neurothekeoma - a benign cutaneous tumor of neural origin. Am J Clin Pathol 1980;74:759-64. [PubMed]2. Allen PW. Myxoma is not a single entity: a review of the concept of myxoma. Ann Diagn Pathol 2000;4:99-123. [PubMed]
3. Benbenisty KM, Andea A, Metcalf J, Cook J. Atypical cellular neurothekeoma treated with Mohs micrographic surgery. Dermatol Surg 2006;32:582-7. [PubMed]
4. Fetsch JF, Laskin WB, Hallman JR, Lupton GP, Miettinen M. Neurothekeoma: an analysis of 178 tumors with detailed immunohistochemical data and long-term patient follow-up information. Am J Surg Pathol 2007;31:1103-14. [PubMed]
5. Mentzel T. Cutaneous neural neoplasms - an update [German]. Pathologe 1999;20:98-109. [PubMed]
6. Page RN, King R, Mihm MC, Googe PB. Microphthalmia transcription factor and NKI/C3 expression in cellular neurothekeoma. Mod Pathol 2004;2:230-4. [PubMed]
7. Laskin WB, Fetsch JF, Miettinen M. The "neurothekeoma": immunohistochemical analysis distinguishes the true nerve sheath myxoma from its mimics. Hum Pathol 2000;31:1230-41. [PubMed]
8. Misago N, Satoh T, Narisawa Y. Cellular neurothekeoma with histiocytic differentiation. J Cutan Pathol 2004;31:568-572. [PubMed]
9. Fullen DR, Lowe L, Su LD. Antibody to S100a6 protein is a sensitive immunohistochemical marker for neurothekeoma. J Cutan Pathol 2003;30:118-22. [PubMed]
10. Hornick JL, Fletcher CD. Cellular neurothekeoma: detailed characterization in a series of 133 cases. Am J Surg Pathol 2007;31:329-40. [PubMed]
11. Avninder S, Ramesh V, Vermani S. Benign nerve sheath myxoma (myxoid neurothekeoma) in the leg. Dermatol Online J 2007;13:14. [PubMed]
12. Peters Jr GE, Wentzell M. Cellular neurothekeoma treated with Mohs micrographic surgery. Dermatol Surg 2007;33:239-44. [PubMed]
13. Ward JL, Prieto VG, Joseph A, Chevray P, Kronowitz S, Sturgis EM. Neurothekeoma. Otolaryngol Head Neck Surg 2005;132:86-9. [PubMed]
© 2009 Dermatology Online Journal