Pityriasis rubra pilaris, type 1
Published Web Location
https://doi.org/10.5070/D39fp4v8h3Main Content
Pityriasis rubra pilaris, type 1
Alexandria V Booth MD and Linglei Ma MD PhD
Dermatology Online Journal 11 (4): 9
Department of Dermatology, New York University School of Medicine
Abstract
A 57-year-old woman presented with a history of dry skin with an associated sensation of burning and itching. It had been previously diagnosed as psoriasis. Clinical and histopathologic examination were consistent with pityriasis rubra pilaris, and treatment consisted of acitretin and narrow-band ultraviolet B phototherapy. Pityriasis rubra pilaris is a papulosquamous disorder of unknown etiology, which can be treated with retinoids, methotrexate, cyclosporine, and narrow-band phototherapy.
A 59-year-old woman was referred to the Charles C. Harris Skin and Cancer Pavilion in October 2002 for the treatment of psoriasis. She noted shedding of dry, flaky skin from the trunk and extremities, burning and itching of her thighs, and a receding hairline. Current treatment consisted of soap and emollients. The diagnosis was confirmed by biopsy, and the patient was treated with fexofenadine and acitretin with moderate improvement. She began narrow-band ultraviolet-B phototherapy in December 2003, with improvement. The patient also had a trial of cyclosporin without change in her disease. Medical history included glaucoma. Prick skin testing showed a positive reaction to ragweed.

|

|
| Figure 1 | Figure 2 |
|---|
|
| Figure 3 |
|---|
Physical examination revealed multiple, hyperkeratotic, follicular, erythematous papules and plaques present on the chest, abdomen, back, buttocks, and upper and lower extremities. On the dorsal and palmoplantar surfaces were scale and fissures. Alopecia with scale was present on the frontal areas and vertex of the scalp. Subungual scale with a thick nail plate and horizontal pigmentation was present on the fingers and toes.
A complete blood count, comprehensive metabolic panel, liver function tests, and lipid panel were normal.
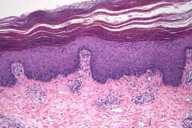
There is epidermal hyperplasia with broad rete ridges, thick suprapapillary plates, a preserved granular layer, and alternating orthokeratosis and parakeratosis in a vertical and horizontal pattern. There are a few dilated blood vessels in the papillary dermis and a superficial perivascular, lymphocytic infiltrate.
Comment
Pityriasis rubra pilaris is a papulosquamous disorder of unknown cause that is characterized by follicular hyperkeratosis, perifollicular erythema and that may progress to generalized erythroderma, and palmoplantar hyperkeratosis. Lesions are characteristically orange or yellow, with approximately 1-cm islands of sparing. Nail findings include longitudinal ridges, subunugual hyperkeratosis, and splinter hemorrhages [1].
Five types of pityriasis rubra pilaris have been described, which differ with respect to age, clinical features, course, and prognosis. The five types include the classic adult and juvenile types (I and III), the atypical adult and juvenile types (II and V), and the circumscribed juvenile type (IV) [2].
Pityriasis rubra pilaris can be difficult to distinguish from psoriasis. Histopathologic features predictive of pityriasis rubra pilaris include follicular plugs, an increased granular-cell layer, and acantholysis. Other features include epidermal atrophy, dermal infiltrates of eosinophils and plasma cells, an abnormal granular-cell layer, and epidermolytic hyperkeratosis although none of these features were statistically significant predictors of pityriasis rubra pilaris over psoriasis [3].
Treatment options include oral retinoids, methotrexate, cyclosporine, and phototherapy. In a study of patients with classic adult-type pityriasis rubra pilaris [1], ten of fifteen patients treated with isotretinoin had complete clearing and two had partial clearing. Four of six patients treated with etretinate had clearing, and all eight patients treated with methotrexate had a favorable response. In patients with juvenile pityriasis rubra pilaris, isotretinoin was associated with the best response in a retrospective study. Treatment with narrow-band ultraviolet B light in combination with acitretin has shown almost complete resolution with flaring when phototherapy was discontinued in one case report [5]. Cyclosporine with or without other treatments has also shown some evidence of improving the disease [6].
References
1. Dicken CH. Treatment of classic pityriasis rubra pilaris. J Am Acad Dermatol 1994;31:9972. Griffiths WAD. Pityriasis rubra pilaris. Clin Exp Dermatol 1980;5:105
3. Magro CM, et al. The clinical and histomorphological features of pityriasis rubra pilaris: a comparative analysis with psoriasis. J Cut Pathol 1997;24:416
4. Allison DS, et al. Pityriasis rubra pilaris in children. J Am Acad Dermatol 2002;47:386
5. Kirby B, et al. Pityriasis rubra pilaris treated with acitretin and narrow-band ultraviolet B. Br J Dermatol 2000;147:376
6. Usuki K, et al. Three cases of pityriasis rubra pilaris successfully treated with cyclosporin A. Dermatology 2000;200:324
© 2005 Dermatology Online Journal

