A case of disseminate and recurrent infundibulofolliculitis responsive to treatment with topical steroids
Published Web Location
https://doi.org/10.5070/D39ct798f5Main Content
A case of disseminate and recurrent infundibulofolliculitis responsive to treatment with topical steroids
Ginette A Hinds MD, Peter W Heald MD
Dermatology Online Journal 14 (11): 11
Yale University Department of Dermatology. ginette.hinds@yale.eduAbstract
Disseminate and recurrent infundibulofolliculitis (DRIF) is an uncommon pruritic follicular eruption of unknown etiology that is predominantly seen in black men. This condition tends to affect the trunk and upper extremities and is usually unresponsive to local and systemic treatment. Recently, several investigators have reported successful treatment with isotretinoin. Herein, we report a case of a patient with disseminate and recurrent infundibulofolliculitis who was successfully treated with potent topical corticosteroids.
Case report
A 65-year-old African American man with a past medical history significant for hypertension and prostate cancer presented to the dermatology clinic with a chief complaint of intractable pruritus of his back. He reported a 40-year history of recurrent episodes of small, itchy lesions on his upper back and shoulders, with severe flares during the summer months.
He used various home remedies over the years with no improvement, including over the counter anti-itch lotions and rubbing alcohol. He had no history of renal failure, liver disease, or anemia. His medications included aspirin, atenolol, hydrochlorothiazide, felodipine, and simvastatin. He had no medication allergies. He denied a personal or family history of atopic dermatitis, asthma, or hayfever. His review of systems was negative.
 |  |
| Figure 1 | Figure 2 |
|---|---|
| Figures 1 & 2. 1 to 2 mm skin-colored follicular papules and pustules on the upper back. Note the background of xerosis and lichenification. | |
On physical exam, he was noted to have widespread 1 to 2 mm skin-colored follicular papules on the upper back, shoulders, and upper chest. The papules could not easily be removed by scratching. They were rounded and uniformly distributed over the affected areas. There were also lichenified plaques and fine scaling on the upper back and shoulders. Scattered 1-2 mm follicular pustules were also noted on his upper chest and back. Unaffected parts of his skin were xerotic and there was no pruritus or evidence of dermatitis on his hands or in his antecubital or popliteal fossae.
The differential diagnosis of this eruption included papular eczema, keratosis pilaris, bacterial folliculitis, pityrosporum folliculitis, lichen planus follicularis, and disseminate and recurrent infundibulofolliculitis.
A potassium hydroxide preparation did not show any fungal hyphae or yeast forms. A Gram stain of material from the pustules on his back showed no organisms. Complete blood count, liver, and renal function tests were within normal limits.
 |
| Figure 3 |
|---|
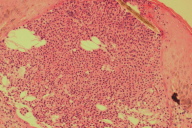
| Figure 3. Dense lymphocytic infiltration of the infundibular portion of the hair follicle (H&E, original magnification x40) |
Histological examination of a punch biopsy specimen taken from his upper back showed lymphocytic infiltration of the infundibular portion of the hair follicle. There were foci of fibrinoid necrosis with adjacent collections of neutrophils at the infundibular orifice. There was no spongiosis in the adjacent epidermis. Stains for yeasts and fungi were negative.
Discussion
The combination of clinical and histopathologic findings, as well as the clinical course supported a diagnosis of disseminate and recurrent infundibulofolliculitis. The differential diagnosis of papular eczema was considered. However, this diagnosis was thought to be less likely given the lack of a personal or family history of atopic dermatitis, asthma, or hayfever and the lack of epidermal spongiosis on histopathology.
Disseminate and recurrent infundibulofolliculitis (DRIF) was first described in 1968 by Hitch and Lund [1]. It is an uncommon eruption characterized by recurrent, pruritic follicular papules on the trunk and proximal extremities. Disseminate and recurrent infundibulofolliculitis is seen more often in black patients. However, a few cases of DRIF in patients of other ethnicities have been described [2, 3].
The etiology of DRIF is unknown. Some authors propose that DRIF represents a pattern of atopic dermatitis in black patients [4], but this hypothesis has been refuted given the lack of personal or family history of atopy in many patients [5]. Others classify DRIF as a form of follicular eczema, along with lichen spinulosus and juxtaclavicular beaded lines [4]. Despite its possible relationship to atopic dermatitis and follicular eczema, DRIF has been anecdotally reported to be unresponsive to systemic, intralesional, and topical steroids [5].
It has also been suggested that the pruritus and lymphocytic spongiosis seen on histology could suggest a delayed hypersensitivity response within the follicle [5], but in most patients the history does not suggest an exogenous contactant.
Disseminate and recurrent infundibulofolliculitis is often resistant to treatment. Bland topical agents, antihistamines, tetracyclines, keratolytics, and topical retinoic acid have been reported to be ineffective. There have been mixed results with oral vitamin A alone and in combination with vitamin E [3, 5]. In the cases described by Owen et al. [5], triamcinolone cream and other unspecified topical steroids were ineffective. Several recent reports describe DRIF responding to isotretinoin [2, 3, 4] and psoralen plus UVA [6].
Our patient applied fluocinonide cream daily for two months. At his two month follow-up visit, he reported a dramatic improvement in his pruritus and the papules, pustules, and lichenification on his back were resolved. He continues to use fluocinonide once weekly for maintenance and has been pruritus and lesion-free for one year.
A high potency steroid in an emollient base, used for 8 weeks, followed by weekly applications was effective in the treatment of DRIF in our patient.
References
1. Hitch JM, Lund HZ. Disseminate and recurrent infundibulo-folliculitis: Report of a case. Arch Dermatol. 1968 Apr;97(4):432-5. PubMed.2. Aroni K, Grapsa A, Agapitos E. Disseminate and recurrent infundibulofolliculitis: response to isotretinoin. J Drugs Dermatol. 2004 Jul-Aug;3(4):434-5. PubMed.
3. Aroni K, Aivaliotis M, Davaris P. Disseminated and recurrent infundibular folliculitis (D.R.I.F): Report of a case successfully treated with isotretinoin. J Dermatol. 1998 Jan;25(1):51-3. PubMed.
4. Calka, O, Metin A, Ozen, S. A case of disseminated and recurrent infundibulofolliculitis responsive to treatment with systemic isotretinoin. J Dermatol. 2002 Jul;29(7):431-4. PubMed.
5. Owen WR, Wood C. Disseminate and recurrent infundibulofolliculitis. Arch Dermatol. 1979 Feb;115(2):174-5. PubMed.
6. Ravikumar, BC, Balachandran C, Shenoi SD et al. Disseminate and recurrent infundibulofolliculitis: response to psoralen plus UVA therapy. Int J Dermatol. 1999 Jan;38(1):75-6. PubMed.
© 2008 Dermatology Online Journal

