Mucoceles not – Oral cysticercosis and minor salivary gland adenocarcinoma: Two case reports
Published Web Location
https://doi.org/10.5070/D392v3948cMain Content
Mucoceles not – Oral cysticercosis and minor salivary gland adenocarcinoma: Two case reports
Kristyna H Lee MD MPH1, Laura Cepeda MD2, Michael Miller MD3, Daniel M Siegel MD MS1
Dermatology Online Journal 15 (7): 8
1. Department of Dermatology, SUNY Downstate Medical Center, Brooklyn, New York. kristynalee.md@gmail.com2. Department of Dermatology, SUNY Downstate Medical Center, Brooklyn, New York
3. Dermpath Diagnostics
Abstract
A mucocele is one of the more commonly encountered disorders of the oral mucosa. It develops when a minor salivary duct is injured or blocked, resulting i n the escape of mucus into the adjacent submucosal connective tissue. We present two cases that were clinically diagnosed as mucoceles that were removed because of patient anxiety. However, histological examination revealed dissimilar and medically significant pathologies. Oral cysticercosis and salivary gland adenocarcinoma are rare diseases of the oral mucosa. It is important to consider these and other uncommon diagnoses when evaluating an oral nodule presumed to be a mucocele. We will discuss the natural history and pathogenesis of these disease processes.
Case report 1
A healthy 38-year-old man was referred for evaluation of multiple intraoral nodules. The lesions were firm, painless, and not related to any traumatic episode. The nodules appeared one year after traveling to Puerto Rico and six months after traveling to Costa Rica. A large solitary nodule arose first followed by three smaller nodules six months later that developed around the primary lesion. The patient had no headaches, seizures or any neurological deficits.
On examination, all nodules were smooth and well defined with intact overlying mucosa. An 8 x 6 mm nodule and three surrounding 3 x 3 mm nodules were seen on the lower labial mucosa (Fig. 1). Clinically, the nodules resembled mucoceles. An excisional biopsy was performed on the largest nodule.
 | 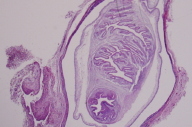 |
| Figure 1 | Figure 2 |
|---|
Histopathological examination revealed a cystic space containing a Cysticercus larva surrounded by a double-layered membrane and connective tissue capsule (Fig. 2). The cephalic end of the larvae revealed an invaginated scolex (Fig. 3). The caudal end of the larva revealed duct-like invaginations lined by a homogenous membrane (Fig. 4). The diagnosis of oral cysticercosis was made.
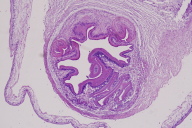 | 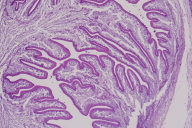 |
| Figure 3 | Figure 4 |
|---|
MRI showed no evidence of cysticerci in the brain or eye. Examination of stool showed no ova, cysts, or parasites. The lesions resolved after an oral course of albendazole 400 mg twice daily.
Cysticercosis discussion
Endemic throughout Latin America, India, Southeast Asia, China, and sub-Saharan Africa, cysticercosis is a parasitic infestation by the larval stage of the pork tapeworm Taenia solium. Humans are the definitive host of T. solium, which live in the human intestinal tract and lay eggs that are shed in human feces. During the normal life cycle of the parasite, eggs shed in human feces are ingested by pigs, which then develop cysticerci in muscle tissue. Human infection with the adult tapeworm then develops when humans ingest raw or poorly cooked pork that contain cysticerci [2, 3, 4, 5].
Infections with cysticercosis may involve many parts of the body including the subcutaneous tissues, eye, heart, liver, lungs, and peritoneum. However, the most commonly affected site is skeletal muscle; the most common site of severe symptomatic infection is the CNS [2, 3, 4, 5]. In spite of the abundance of muscular tissue in the oral and maxillofacial regions, this is not a frequent site of occurrence for cysticercosis. When present, the most frequently involved oral locations are the tongue, labial or buccal mucosa, and mouth floor [3, 4, 5].
The most common complaint by patients is swelling. Pain is not a frequent feature unless secondarily infected. Lesions on the tongue could interfere with movement, causing discomfort during speaking and eating. Most oral presentations are in the form of painless, well-circumscribed, soft swellings that may mimic fluctuant lesions like mucoceles [2, 3, 4, 5]. Clinical differential diagnoses depend on the site involved and include retention cysts, lipomas, fibromas, neurofibromas, and mucoceles [2].
Histopathological examination confirms a diagnosis of cysticercosis by the detection of a cystic space containing the Cysticercus cellulosae. A duct-like, invaginated segment, lined by a homogenous anhistic membrane, composes the caudal end. The eosinophilic membrane that lines the capsule is double-layered, consisting of an outer acellular and inner sparsely cellular layer.
The diagnosis of oral cysticercosis is made by serology or direct histological examination. Computerized tomography (CT) and magnetic resonance imaging (MRI) may be used to evaluate for CNS involvement [3, 4, 5].
Treatment of oral cysticercosis must be tailored to the specific needs of the patient and relies on antihelminthic drugs or surgery [6].
Case report 2
A 71-year-old woman with a 30-pack-year history of cigarette smoking was referred for evaluation of a slowly enlarging painless intraoral lump present for five years. Examination revealed a solitary 3 x 3 mm freely mobile, smooth, firm nodule on the labial mucosa of the upper lip. The clinical diagnosis was a mucocele, which was surgically excised at the patient's request.
 |  |
| Figure 5 | Figure 6 |
|---|
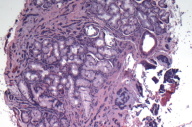
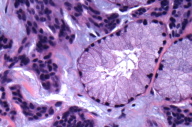
Histopathological examination revealed a proliferation of epithelial cells forming nests, cords, and strands of infiltrate within a hyalinized stroma surrounding a minor salivary gland (Fig. 5). On high power, tumor cells infiltrate as strands within a mucinous stroma surrounding a minor salivary gland (Fig. 6).
The diagnosis of polymorphous low-grade adenocarcinoma of a minor salivary gland was made. Mohs micrographic surgery was performed and no residual carcinoma was identified in the Mohs stage. On follow-up, she is doing well without evidence of further disease.
Salivary gland adenocarcinoma discussion
The minor salivary glands include approximately 500 – 1000 simple tuboalveolar glands distributed throughout the mucosa of the lips and cheeks, hard and soft palate, uvula, floor of mouth, posterior tongue, and peritonsilar area. The largest concentration is found on the hard palate [7]. These glands are predominately mucous secreting and produce most of the saliva not secreted at mealtime. They moisten and protect mucous membranes by facilitating taste deglutition and guarding against cavities.
Fifteen to twenty-three percent of minor salivary gland neoplasms are malignant [8]. Polymorphous low-grade adenocarcinoma (PLGA) is a malignant tumor that accounts for 7 – 11 percent of all tumors in minor salivary glands [7]. PLGA has low aggressiveness and a generally good prognosis with recurrence rates from 17 – 24 percent [8].
Risk factors associated with the development of salivary gland neoplasms include positive family history of salivary gland cancer, radiation exposure from radiotherapy, and occupational exposure in wood workers, asbestos miners, rubber manufacturers, and plumbers. Interestingly, unlike other cancers of the head and neck, smoking tobacco and consuming alcohol are not clearly linked to increased risk of salivary gland carcinoma [7].
Most salivary gland neoplasms occur in the third to fifth decade of life and have a slight female predominence. Symptoms are based on location. Pain, dysphagia, parasthesias, and speech impairment may occur depending on the size and location of the tumor. Most frequently on physical exam, patients complain of a slow-growing painless mobile nodule covered by smooth mucosa that can reach sizes between 1 and 4 cm [10].
Adenocarcinomas display heterogeneous histology, but the presence of glands and the absence of epidermoid differentiation is common to all lesions. Histopathological examination reveals a focally infiltrative neoplasm with a proliferation of epithelial cells forming nests cords and strands embedded in a fibrous stroma surrounding a minor salivary gland. A variety of growth patterns are present within the same lesion of a PLGA. It is named polymorphous because of its different growth patterns: tubular, solid, papillary, microcystic, cribiform, fascicular, and in cords. Polymorphous low-grade adenocarcinoma can also infiltrate bone tissue and show perivascular and perineural invasion [9].
Treatment for salivary gland adenocarcinoma include conservative but complete surgical excision and/or neck dissection given clinical evidence of cervical lymph node metastasis [10].
In summary, not all small oral cystic lesions are banal and biopsy is a valuable tool to be considered if any uncertainty exists.
References
1. Baurmash HD. Mucoceles and ranulas. J Oral Maxillofac Surg 2003;61:369-378. [PubMed]2. Garcia HH, Del Brutto OH. Taenia solium cysticercosis. Infect Dis Clin North Am 2000;14:97-119 [PubMed]
3. de Souza PE, Barreto DC, Foneseca LM, de Paula AM, Silva EC, Gomez RS. Cysticercosis of the oral cavity: report of seven cases. Oral Dis 2000;6:253-5. [PubMed]
4. Ribeiro AC, Luvizotto MC, Soubhia AM, de Castro AL. Oral cysticercosis: case report. Oral Surg Oral Med Oral PAthol Oral Radiol Endod. 2007 Oct;104(4):e56-8. [PubMed]
5. Sara RK, Rattan V, Rajwanshi A, Nijkawan R, Gupta SK. Cysticercosis of the oral cavity: report of five cases and review of literature. Int J Paediatr Dent 1998;8:273-8 [PubMed]
6. White, Jr., A. Clinton. New developments in the management of neurocysticercosis. J Infect Dis 2009;199:1261. [PubMed]
7. Ellis GL, Auclair PL. Atlas of tumor pathology: tumors of the salivary glands. Washington, DC: Armed Forces Institute of Pathology; 1996.
8. Gonzalez LJ, Rodado C, Raspall G, Bermejo B, Huguet P, Giralt J. Malignant tumors of the minor salivary glands: retrospective study on 59 cases. Med Oral 2001;6(2):142-7 [PubMed]
9. Darling MR, Schneider JW, Phillips VM. Polymorphous low-grade adenocarcinoma and adenoid cystic carcinoma: a review and comparison of immunohistochemical markders. Oral Onc 2002;38:641-5 [PubMed]
10. Pintor MA, Figueroa L, Martinez B. Polymorphous low-grade adenocarcinoma: review and case report. Med Oral Patol Oral Cir Buscal 2007;12(8):E549-51. [PubMed]
© 2009 Dermatology Online Journal

