Cowden syndrome
Published Web Location
https://doi.org/10.5070/D3916821pqMain Content
Cowden syndrome
Marcio A Oliveira, Janaina B Medina, Flavia C Xavier, Marina Magalhães, Karem L Ortega PhD
Dermatology Online Journal 16 (1): 7
Department of Oral Pathology, Special Care Dentistry Center, University of São Paulo, Brazil. klortega@usp.brAbstract
Mucocutaneous papillomas can be manifestations of an autosomal dominant condition known as Cowden syndrome (CS). We report the case of a 22-year-old man with oral and cutaneous papules and a past history of thyroid malignancy. It is important to recognize oral manifestations of CS; they can lead to early diagnosis of the condition.
Case report
 |  |
| Figure 1 | Figure 2 |
|---|---|
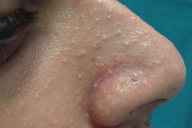
| Figure 1. Multiple white, smooth papules spread over the lower lip Figure 2. Smaller papules were seen in the area around the nose | |
A 22-year-old man presented with a complaint of multiple papules on the lips, which had been noticed the previous year. Physical examination revealed macrocephaly, and many white, smooth papules spread over the lower lip.
 |  |
| Figure 3 | Figure 4 |
|---|---|
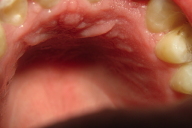
| Figure 3. Additional lesions were found on the tongue Figure 4. Lesions on the maxillary gingiva (palate) | |
Additional lesions were found on the tongue, maxillary gingiva, alveolar mucosa and both sides of the buccal mucosa. The patient's past medical history revealed a thyroid cancer, which had been removed when he was 15 years old. His father had also presented with the same type of tumor at the same age. Biopsies were performed of the lip, gingiva, and buccal mucosa.
 |  |
| Figure 5 | Figure 6 |
|---|---|
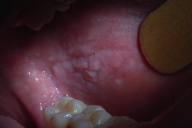
| Figure 5. Lesions on the maxillary gingiva (vestibular, right side) Figure 6. Lesions on the alveolar mucosa | |
 |  |
| Figure 7 | Figure 8 |
|---|---|
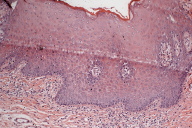
| Figure 7. Lesions on the buccal mucosa Figure 8. Papilliferous oral mucosa with mild epithelial hyperplasia, acanthosis, hyperkeratosis and inflammatory infiltrate (H&E, x20) | |
Histopathologic examination of the biopsy specimen revealed papilliferous oral mucosa with mild epithelial hyperplasia, acanthosis, hyperkeratosis and inflammatory infiltrate. The oral mucosal lesions were diagnosed as benign fibromas.
In order to provide additional support for the diagnosis and to confirm the abnormalities in the PTEN/AKTpathway that constitute the genetic basis of CS, immunohistochemistry for PTEN and p-AKT was performed as described by Scheper et al. (2006) [1]. In essence, paraffin-embedded serial tissue sections of 3 µm in thickness were dewaxed and pretreated for antigen retrieval in 0.01 M Citric-acid buffer. The applied primary antibodies were mouse monoclonal anti-PTEN and anti-p-AKT ser 473 antibodies (Cell Signaling Technologies, Beverly, MA, diluted at 1:50). Immune complexes were treated with a secondary biotinylated antibody (K0690; Biotinylated LinK Universal, LSAB + System-HRP; Dako) and exposed to streptavidin-biotin complex (Streptavidin-HRP, LSAB + System-HRP; Dako). The immunoreactivity was visualized with 3,3'-diaminobenzidine tetrahydrochloride (K3468;Dako) and sections were counterstained with Mayer's hematoxylin. The immunohistochemical analysis of the biopsy specimens showed expression of p-AKT and a decreased expression of PTEN in the nucleus and cytoplasm of the lesional fibroblasts, compared to the vascular endothelial cells used as internal control. The diagnosis of Cowden syndrome was established. Management of lip and oral lesions was carried out by surgical excision for cosmetic purposes. Because Cowden syndrome is related to endocrinologic complications and to the development of malignancies, the patient is being periodically followed-up by a multidisciplinary team.
Discussion
Cowden syndrome (CS) is a rare inherited autosomal dominant genodermatosis, with incomplete penetrance, variable expressivity, and a gene mutation (PTEN-Phosphatase and Tensin Homologue) [2].
PTEN is a tumor-suppressor gene located at 10q23.3, which antagonizes the phosphoinositol-3-kinase (PI3K)/Akt pathway [3, 4]. Mutations of PTEN are associated with hamartoma-neoplasia syndromes [5]. Germline mutations of this gene characterize Bannayan-Riley-Ruvalcaba syndrome (BRRS), Proteus syndrome (PS), Proteus-like syndrome (PLS), and Cowden syndrome (CS) [6]. PTEN gene mutation is present in 80 percent of CS patients, 60 percent of BRRS, 50 percent of PLS, and 22 percent of PS patients [3, 7]. The mutational spectrum of CS and BRRS overlap exhibits many of the mutations occurring in exons 5, 7, and 8 [6].
Genetic examination for germline mutations of the PTEN gene in CS can be performed by PTEN mutation analysis of all nine coding exons, exon-intron junctions, and flanking intronic sequences using PCR-based denaturing gradient gel electrophoresis and semiautomated sequencing [8, 9].
Because a mutation in the PTEN gene can promote a premature stop codon in the protein, immunohistochemistry is becoming an interesting technique that can provide additional support for the diagnosis and confirm the abnormalities in the PTEN/AKTpathway that constitute the genetic basis of CS [1].
The diagnosis of CS has been facilitated by the establishment of the International Cowden Consortium, which proposed a set of operational diagnosis criteria divided into pathognomonic lesions (facial trichilemmomas, acral keratosis, papillomatous papules, and mucous lesions), major criteria (mammary carcinoma, thyroid carcinoma, macrocephalia, Lhermitte-Duclos disease, and endometrial carcinoma) and minor criteria (other thyroid pathology, mental retardation, intestinal hamartomatous polyps, fibrocystic mammary disease, lipomas, fibromas, urogenital tumors, and urogenital malformations) [10].
Cowden syndrome is diagnosed when the patient shows the presence of 1) pathognomonic lesions, (six or more facial papules, of which three or more must be trichilemmomas; facial papules and papillomatosis in oral mucosa; papillomatosis in oral mucosa and acral keratosis; six or more palmoplantar keratosis lesions); 2) presence of two major criteria, one of which must be macrocephalia or Lhermitte-Duclos disease; 3) presence of one major criterion and three minor criteria; 4) presence of four minor criteria [10].
Most CS affected people develop these characteristic lesions by the age of 20 years [9]. Once the diagnosis of Cowden syndrome is made, patients have to be considered at high risk for developing malignancies [12].
Conclusions
It is important for clinicians to recognize oral manifestations of Cowden syndrome because they can lead to the early diagnosis of the condition.
References
1. Scheper MA, Nikitakis NG, Sarlani E, Sauk JJ, Meiller TF. Cowden syndrome: report of a case with immunohistochemical analysis and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101(5):625-31. [PubMed]2. Botma M, Russell DI, Kell RA. Cowden's disease: a rare cause of oral papillomatosis. J Laryngol Otol. 2002;116(3):221-3. [PubMed]
3. Zhou XP, Waite KA, Pilarski R, Hampel H, Fernandez MJ, Bos C, Dasouki M,Feldman GL, Greenberg LA, Ivanovich J, Matloff E, Patterson A, Pierpont ME, Russo D, Nassif NT, Eng C. Germline PTEN promoter mutations and deletions in Cowden / Bannayan-Riley-Ruvalcaba syndrome result in aberrant PTEN protein and dysregulation of the phosphoinositol-3-kinase/Akt pathway. Am J Hum Genet. 2003;73(2):404-11. [PubMed]
4. Schaffer JV, Kamino H, Witkiewicz A, McNiff JM, Orlow SJ. Mucocutaneous neuromas: an underrecognized manifestation of PTEN hamartoma-tumor syndrome. Arch Dermatol. 2006;142(5):625-32. [PubMed]
5. Reardon W, Zhou XP, Eng C. A novel germline mutation of the PTEN gene in a patient with macrocephaly,ventricular dilatation, and features of VATER association. J Med Genet. 2001;38(12):820-3. [PubMed]
6. Eng C. PTEN: one gene, many syndromes. Hum Mutat. 2003;22(3):183-98. [PubMed]
7. Zhou X, Hampel H, Thiele H, Gorlin RJ, Hennekam RC, Parisi M, Winter RM, Eng C. Association of germline mutation in the PTEN tumour suppressor gene and Proteus and Proteus-like syndromes. Lancet. 2001. 358:210-1. [PubMed]
8. Mutter GL, Lin MC, Fitzgerald JT, Kum JB, Baak JP, Lees JA, et al. Altered PTEN expression as a diagnostic marker for the earliest endometrial precancers. J Natl Cancer Inst 2000, 92:924-930. [PubMed]
9. Marsh DJ, Roth S, Lunetta KL, Hemminki A, Dahia PL, Sistonen P, et al. Exclusion of PTEN and 10q22-24 as the susceptibility locus for juvenile polyposis syndrome. Cancer Res 1997, 57:5017-5021. [PubMed]
10. Eng C. Will the real Cowden syndrome please stand up: revised diagnostic criteria. J Med Genet. 2000;37(11):828-30. [PubMed]
11. Jornayvaz FR, Philippe J. Mucocutaneous papillomatous papules in Cowden's syndrome. Clin Exp Dermatol. 2008;33(2):151-3. [PubMed]
12. Leão JC, Batista V, Guimarães PB, Belo J, Porter SR. Cowden's syndrome affecting the mouth, gastrointestinal, and central nervous system: a case report and review of the literature.Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99(5):569-72. [PubMed]
© 2010 Dermatology Online Journal

