Keratoacanthoma arising in nevus comedonicus
Published Web Location
https://doi.org/10.5070/D38xz7951sMain Content
Keratoacanthoma arising in nevus comedonicus
Sara Zarkik MD, Jamila Bouhllab MD, Aicha Methqal MD, Yassir Afifi PhD, Karima Senouci PhD, Badreddine Hassam PhD
Dermatology Online Journal 18 (7): 4
Department of Dermatology, Avicenne University Hospital, Rabat, MorroccoAbstract
Nevus comedonicus is a benign hamartoma of the pilosebaceous unit and is considered as a rare subtype of epidermal nevus. It was first described in 1895. It manifests as a group of closely dilated follicular openings with dark keratin plugs resembling comedones. Malignant degeneration of a nevus comedonicus is exceptional; we report a case of keratoacanthoma arising in extensive nevus comedonicus.
Introduction
Nevus comedonicus is a benign hamartoma of the pilosebaceous unit and is considered a rare subtype of epidermal nevus. It was first described in 1895 by Kofmann [1]. It manifests as a group of closely dilated follicular openings with dark keratin plugs resembling comedones. We report the first case of keratoacanthoma arising in extensive nevus comedonicus.
Case report
A 20-year-old man presented with asymptomatic grouped comedo-like keratin filled pits on the right lower limb since his birth. The lesions grew with the patient's growth, but faster during puberty. There was no history of a similar case in the family.
 |  |
| Figure 1 | Figure 2 |
|---|---|
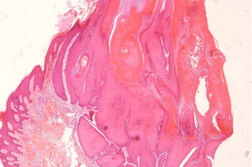
| Figure 1. Linear disposition of nevus comedonicus Figure 2. Keratoacanthoma arising in nevus comedonicus | |
 |
| Figure 3 |
|---|
| Figure 3. Groups of comedo-like keratin filled pits |
Examination revealed multiple groups of dilated pilosebaceous orifices filled with black keratin plugs arranged linearly along the posterior side of the right lower leg. Some cutaneous lesions in the middle of the hamartoma began burgeoning when he was 18 years old. Lesions were asymptomatic, unilateral, and irregularly scattered throughout the skin. The soles, palms, and mucosa were spared and regional lymph nodes were not palpable. The skin biopsy of the budding area revealed a keratoacanthoma.
Because of the size and location of the lesion surgery was not advised for this patient. Therefore, we opted for methotrexate (25 mg intramuscular weekly). Regression of the lesion was observed over two months of treatment.
Discussion
Nevus comedonicus usually arises before the age of 10; it is present at birth in almost half of the cases. The majority of cases are solitary. However, this hamartoma may be part of nevus comedonicus syndrome in association with skeletal anomalies (scoliosis, fused vertebrae, spinabifida occulta, absent fifth finger) or central nervous pathologies (seizures, changes noted on EEG, transverse myelitis), ocular alterations (cataracts) [2], and cutaneous defects (multiple basal cell carcinoma) [3]. Our patient did not have any systemic findings.
Nevus comedonicus is evident clinically as confluent clusters of dilated follicular orifices plugged with keratin, giving the appearance of aggregated open comedones. These clusters are often arranged in a linear or zosteriform pattern, occasionally in parallel with the lines of Blaschko. Although usually unilateral, bilateral occurrences have been noted. As with other epidermal nevi, the most common sites are the face, trunk, and proximal extremities.
The pathogenesis of NC remains obscure. Immunohistochemical studies show that filaggrin is involved in the formation of closed comedones and may be involved in the pathogenesis of abnormal keratinization in nevus comedonicus [4].
Comedo nevus is a benign lesion and does not need treatment unless the patient requires it for aesthetic reasons or has a complication. Treatment options for nevus comedonicus include antibiotics for inflamed or infected lesions, topical keratolytics, topical retinoic acid (0.025% - 0.1%), 12 percent ammonium lactate lotion, calcipotriene, oral retinoids, dermabrasion, superficial shaving, or surgical excision [5, 6]. Also, the use of erbium: YAG [7] and CO2 laser has been reported [8]. Our patient was treated in his childhood by topical retinoids, but without any remarkable improvement.
Epidermal nevus has been associated with benign and malignant neoplasms [9, 10], but malignant degeneration of nevus comedonicus is exceptional. Literature reports only one case of squamous cell carcinoma on a facial nevus comedonicus [11]. The present case is characterized by the appearance of keratoacanthoma in a very extensive nevus comedonicus. Keratoacanthoma is a fairly common neoplasm among light-skinned people. It was once considered a pseudomalignancy that resembled squamous cell carcinoma. It is now considered to be a squamous cell carcinoma that resembles a pseudo-benign tumor [12]. Our patient responded well to methotrexate.
Conclusion
From this paper and based on this case we recommend a close surveillance of this kind of hamartoma in order to detect malignant degeneration.
References
1. Kofmann et al., a case of rare localization and spreading of comedones. Arch Dermatol Syphilol 1895.2. El Ghelbazouri N, Ismaili N, Ahrich N, Benarafa A, Senouci K, Mansouri F, Hassam B.Nevus comedonicus syndrome. Ann Dermatol Venereol. 2007 Aug-Sep;134(8-9):663-6. [PubMed]
3. Erkan et al., Nevus comedonicus syndrome: a case associated with multiple basal cell carcinomas and a rudimentary toe. International Journal of Dermatology 2005. [PubMed]
4. Kurokawa I, Nakai Y, Nishimura K, Hakamada A, Isoda K, Yamanaka K, Mizutani H, Tsubura A. Cytokeratin and filagrinn expression in nevus comedonicus. J Cutan Pathol. 2007; 34: 338-41. [PubMed]
5. Lefkowitz A, Schwartz RA, Lambert WC. Nevus comedonicus. Dermatology. 1999;199:204-7. [PubMed]
6. Deliduka SB, Kwong PC. Treatment of nevus comedonicus with topical tazarotene and calcipotriene. J Drugs Dermatol 2004;3:674-6. [PubMed]
7. Caers SJ, Van der Geer S, Beverdam EG, Krekels GA, Ostertag JU. Successful treatment of nevus comedonicus with the use of the Erbium Yag laser. J Eur Acad Dermatol Venereol. 2008; 22: 375-7. [PubMed]
8. Sardana K, Garg VK. Successful treatment of nevus comedonicus with ultrapulse CO2 laser. Indian J Dermatol Venereol Leprol. 2009;75:534-5. [PubMed]
9. Vidaurri-de la Cruz H, Tamayo Sanchez L, Duran-McKinester C, Orozco-Covarrubias M, Ruiz-Maldonado R. Epidermal Nevus Syndromes:Clinical Findings in 35 patients. Pediatr Dermatol 2004; 21: 432-9. [PubMed]
10. Vujevich J, Mancini A. The epidermal nevus syndromes: Multisystem Disorders. J Am Acad Dermatol 2004; 50: 957-61. [PubMed]
11. Hobar et al., Squamous Cell Carcinoma Arising in Nevus Comedonicus. Dermatol Surg 2009. [PubMed]
12. Schwartz RA. Keratoacanthoma: A clinico-pathologic enigma. Dermatol Surg. 2004;30:2, Part 2, 326-333. [PubMed]
© 2012 Dermatology Online Journal