Hereditary hidradenitis suppurativa restricted to the auricular region
Published Web Location
https://doi.org/10.5070/D38pt8f7mmMain Content
Hereditary hidradenitis suppurativa restricted to the auricular region
Elizabeth Satter MD MPH
Dermatology Online Journal 18 (11): 8
US Navy, San Diego, CaliforniaAbstract
Hidradenitis suppurativa (HS) is part of the follicular occlusion tetrad, which typically presents as recurrent deep-seated nodules, abscesses, and communicating sinus tracts with a predilection for the axilla and genital region. There is only one prior report of HS restricted to the auricular region. Herein the first familial case of HS restricted to the auricular region is reported.
Case presentation
 |  |
| Figure 1 | Figure 2 |
|---|---|
| Figure 1. Preauricular pits and sinus tract Figure 2: Postauricular cysts and open comedones | |
 |
| Figure 3 |
|---|
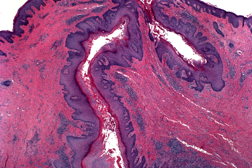
| Figure 3. Sinus tracts lined with epithelium, dermal fibrosis and mixed inflammatory infiltrate |
A 28-year-old male presented with recurrent bilateral painful cysts and sinus tracts, which occasionally drained that had been present since puberty. He was otherwise healthy with no prior history of facial or back acne, pseudofolliculitis barbae, or dissecting scalp folliculitis. He denied smoking and his total body mass index was within normal limits. His father had identical lesions in the same location that presented at puberty and gradually improved with age. On examination, there were erythematous indurated plaques composed of multiple cysts and scattered sinus tracts, admixed with open comedones and shallow pits, in the bilateral periauricular region and on the ear lobes (Figures 1 and 2). No lesions were identified in his axilla or anogenital region. An incisional biopsy was performed from his right postauricular region, which revealed interconnecting epithelial lined sinus tracts and cysts filled with keratin debris (Figure 3). The dermis was fibrotic and contained a mixed inflammatory infiltrate composed of lymphocytes, histiocytes, and plasma cells, with focal collections of neutrophils.
Discussion
Hidradenitis suppurativa is part of the follicular occlusion tetrad, which includes dissecting cellulitis of the scalp, acne conglobata, and pilonidal cysts. Because of their similarities, it has been suggested that acne inversa be used as an all-inclusive term [1]. Since these disorders are considered interrelated entities, patients who present with tender inflamed nodules, recurrent cysts, and interconnecting sinus tracts in any location should prompt a complete physical examination in search for lesions elsewhere.
Although initially considered an apocrine disorder, HS has been shown to represent a chronic and relapsing inflammatory disorder of the pilosebaceous glands. The inciting event is occlusion of the follicular infundibulum, followed by follicular rupture and a vigorous inflammatory response. Pathogenic anaerobes do not contribute to the primary pathogenesis [1].
Clinically, HS is characterized by recurrent deep-seated nodules, abscesses, and communicating sinus tracts that eventuate in dermal fibrosis. Lesions have a predilection for intertriginous areas with the axilla and genital region most commonly involved. Other sites of involvement include the inframammary folds, abdomen, face, external auditory canals, ear lobes, and retroauricular folds [2, 3, 4]. There is only one prior report of HS that was restricted to the auricular region [3].
It has been estimated that HS has a prevalence of 1 percent with most studies showing a female predominance [5]. Men have a greater tendency for atypical locations, more severe disease, and associated acne [5]. Although most cases occur sporadically, a familial form with autosomal dominant inheritance has been reported [1, 4]. Because lesions tend to develop postpubertally, elevated androgen levels were felt to play a role in the pathogenesis; yet, most patients have a normal androgen profile [4]. Some authors hypothesize that the defect lies at the androgen receptor level [4, 6]. Obesity and smoking have been postulated to be contributory factors, but heretofore their role in the development of the lesions has yet to be elucidated.
The severity of HS can be classified using the Hurley clinical staging system [4, 5]. Hurley stage I is defined as having single or multiple abscesses without sinus tracts. Patients with Hurley stage II have recurrent abscesses, sinus tracts, and cicatrization separated by uninvolved skin. Patients with Hurley stage III have more diffuse involvement with multiple interconnected sinus tracts and abscesses. Although there is no single effective treatment for HS, recently, a comprehensive review addressing various treatment options based upon clinical stage has been published [7]. In brief, patients with Hurley stages I and II should receive topical clindamycin, or oral clindamycin in combination with rifampin, respectively. In both stages, various lasers may also be utilized. TNF-alpha inhibitors have been used with some success [2, 7]. For patients with Hurley Stage III or refractory HS, surgical excision is often the best option [7]. Regardless of the treatment, HS remains a chronic condition; treatment is challenging and often disappointing. This case illustrates that HS can be familial and restricted to an atypical location. It should be considered in the differential diagnosis of unusual acne.
References
1. Jansen T, Plewig G. Acne Inversa. Int J Dermatol 1998;37:96-100. [PubMed]2. Moul DK, Korman NJ. Severe Hidradenitis Suppurativa treated with Adalimumab. Arch Dermatol 2006;142:1110-1112. [PubMed]
3. Jain S, Sardana K, Garg VK, Sinha S. Hidradenitis suppurativa involving the preauricular region: An unusual location. Indian J Dermatol Venereol Leprol 2012;78:229-332. [PubMed]
4. Danby FW, Margesson LJ. Hidradenitis suppurativa. Dermatol Clin 2010; 28:779. [PubMed]
5. Canoui-Poitrine F, Revuz JE, Wolkenstein P et al. Clinical characteristics of a series of 302 French patients with hidradenitis suppurativa, with an analysis of factors associated with disease severity. J Am Acad Dermatol 2009;61:51-57. [PubMed]
6. Gee BC, Dawber RP. Hidradenitis Suppurativa. J Royal Soc Med 2000;93:661. [PubMed]
7. Ramnhatla PV, Lim HW, Hamzavi I. A systematic Review of Treatments for Hidradenitis Supurativa. Arch Dermatol. 2012;148:439-446. [PubMed]
© 2012 Dermatology Online Journal

