Acquired smooth-muscle hamartoma
Published Web Location
https://doi.org/10.5070/D38nx15710Main Content
Acquired smooth-muscle hamartoma
Molly Yancovitz MD, Mercedes E Gonzalez MD, Henry J Votava MD, Ruth Walters MD, Roopal Kundu MD, Jerome L Shupack MD
Dermatology Online Journal 15 (8): 12
Department of Dermatology, New York UniversityAbstract
A 52-year-old woman presented with an occasionally pruritic, hyperpigmented and hypertrichotic, indurated plaque on the left upper arm that initially developed during childhood. Histopathologic examination showed changes that were consistent with a smooth-muscle hamartoma. Cutaneous smooth-muscle hamartomas are uncommon benign neoplasms. Most lesions are congenital, but there have been a few reports of acquired lesions. These lesions have been described as part of a spectrum of neoplasms that include Becker nevi since they share many clinical and histopathologic features.
 |  |
| Figure 1 | Figure 2 |
|---|---|
History
A 52-year-old woman presented to the Charles C. Harris Skin and Cancer Pavilion in October, 2008, with a light-brown, indurated plaque on her left arm. The lesion had been present since the age of six and slowly enlarged as the patient grew. The lesion was occasionally pruritic. With heat and sun exposure, it became more pruritic, darker, more indurated, and developed red and white papules within the lesion. Rubbing did not induce any cutaneous changes. She had never treated the lesion. No one in the patient's immediate family had similar lesions. The patient denied any medical problems or medications.
Physical Examination
On the lateral aspect of the left upper arm was a 15 cm, slightly hyperpigmented plaque with hypertrichosis and overlying grouped pink papules.
Laboratory data
None.
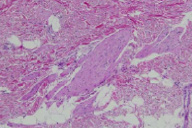
Histopathology
There are haphazardly oriented and thick smooth muscle bundles in the reticular dermis and subcutis.
Comment
Cutaneous smooth-muscle hamartomas are uncommon benign neoplasms that are characterized by an increased density of smooth muscle bundles in the dermis and subcutis. Most lesions are congenital; however, acquired lesions also have been reported [1, 2, 3, 4].
Lesions typically present as indurated, hyperpigmented plaques with hypertrichosis or perifollicular papules. The degree of induration, pigmentation, and hypertrichosis has been noted to change over time [5]. The lesions are most commonly located on the trunk or proximal aspects of the extremities, and some display a pseudo-Darier sign, in which rubbing induces transient piloerection or elevation of the lesion [6]. Pruritus of the lesion has been reported, which included one patient who noted pruritus after hot showers [2, 4].
Histopathologic features include haphazardly-oriented, intradermal bundles of smooth muscle. The bundles can be associated with hair follicles and can extend into the subcutaneous tissue. Acanthosis, hyperkeratosis, and hypermelanomasis may be observed [5].
Smooth-muscle hamartomas are considered by some to be on a continuum with Becker nevi [1], while others classify them as two distinct entities [2, 7]. Cutaneous smooth-muscle hamartomas are more commonly congenital, can be flesh-colored or hyperpigmented, and frequently contain long vellous hairs [3]. In contrast, most Becker nevi are acquired, typically occur around puberty, and display hyperpigmentation, hypertrichosis, and often contain smooth muscle bundles. However, both acquired smooth-muscle hamartomas and congenital Becker nevi have been reported, and thus there is some controversy as to how to distinguish between these entities.
The clinical differential diagnosis of a smooth-muscle hamartoma includes congenital nevocellular nevus, Becker nevus, café-au-lait macule, epidermal nevus, leiomyoma, connective-tissue nevus, and solitary mastocytoma. Histopathologic evaluation is necessary for definitive diagnosis.
Isolated smooth muscle hamartomas have not been associated with systemic diseases nor do they appear to have malignant potential [7, 8]. Thus treatment of smooth-muscle hamartomas is not necessary; however, surgical excision can be undertaken if desired. Smooth muscle hamartomas have been identified as the underlying lesion in a few cases of the Michelin tire baby syndrome [9, 10].
References
1. Wong RC, et al. Acquired dermal smooth-muscle hamartoma. Cutis 1985; 35: 369 [PubMed]2. Darling TN, et al. Acquired cutaneous smooth muscle hamartoma. J Am Acad Dermatol 1993; 28: 844 [PubMed]
3. Morales-Callaghan A, et al. Acquired cutaneous smooth muscle hamartoma. J Eur Acad Dermatol Venereol 2005; 19: 142 [PubMed]
4. ul Bari A, et al. Acquired smooth muscle hamartoma. Indian J Dermatol Venereol Leprol 2006; 72: 178 [PubMed]
5. Holst VA, et al. Cutaneous smooth muscle neoplasms: clinical features, histologic findings, and treatment options. J Am Acad Dermatol 2002; 46: 477 [PubMed]
6. Johnson MD, et al. Congenital smooth muscle hamartoma: report of six cases and a review of the literature. Arch Dermatol 1989; 125: 820 [PubMed]
7. Gagne EJ, et al. Congenital smooth muscle hamartoma of the skin. Pediatr Dermatol 1993; 10: 142 [PubMed]
8. Zarineh A, et al. Smooth muscle hamartoma associated with a congenital pattern melanocytic nevus, a case report and review of the literature. J Cutan Pathol 2008; 35 (Suppl 1):83 [PubMed]
9. Glover MT, et al. Michelin-tire baby syndrome resulting from diffuse smooth muscle hamartoma. Pediatr Dermatol 1989; 6: 329 [PubMed]
10. Schnur RE, et al. Variability in the Michelin tire syndrome: child with multiple anomalies, smooth muscle hamartoma, and familial paracentric inversion of chromosome 7q. J Am Acad Dermatol 1993; 28: 364 [PubMed]
© 2009 Dermatology Online Journal

