Mycobacterium marinum infection
Published Web Location
https://doi.org/10.5070/D38g69t02kMain Content
Mycobacterium marinum infection
Christopher T Cassetty MD, and Miguel Sanchez MD
Dermatology Online Journal 10 (3): 21
From the Ronald O. Perelman Department of Dermatology, New York University
Abstract
A 49-year-old man presented with nodules on his right hand after a history of Mycobacterium marinum infection recently treated with rifampin and clarithromycin. The patient has an aquarium with Betta fish (Siamese fighting fish).
Clinical synopsis
History.—A 49 year-old man presented to the Dermatology Clinic at Bellevue Hospital Medical Center in April 2004 with a tender nodule on the dorsum of his right hand. There was no drainage or pain, but the lesion slowly enlarged over 3 weeks. In the fall of 2003, a nodular eruption extended from his right third fingertip proximally along his right forearm. This eruption was biopsied and cultured. Multiple antibiotics were initiated that included amoxicillin-clavulanate, levofloxacin, clindamycin, cephalexin, and minocycline. Rifampin and clarithromycin were administered, and the nodules resolved but reappeared on the dorsal aspect of the hand 3 months later. A new antibiotic regimen of gatifloxacin and clarithromycin was started. The patient has a pair of Betta fish (Betta splendens, Siamese fighting fish) at home, but he wears gloves when cleaning the tank.
Past medical history includes diabetes mellitus and coronary artery disease. Current medications include glipizide, rosiglitazone/metformin, quinapril, and atorvastatin.
Physical examination.— On the right, dorsal, third, metacarpophalangeal joint there were three, erythematous, tender, exophytic nodules approximately 0.5-to-1.0-cm in size. There were lichenification and scale but no ulcers. Lymphadenopathy was not present.

|

|
| Figure 1 | Figure 2 |
|---|
|
| Figure 3 |
|---|
Laboratory data.—In December 2003, a culture grew Mycobacterium marinum that was sensitive to kanamycin, ethionamide, ansamycin, and ciprofloxacin and resistant to isoniazid, streptomycin, rifampin, para-amino salicyclic acid, and ethambutol. Cultures were negative for bacteria and fungi.
In April 2004, a radiograph of the right hand showed soft tissue swelling over the third metacarpal head without bony involvement; the second and third metacarpal joint spaces may be narrowed.
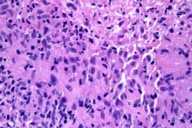
Histopathology.—In the deep reticular dermis, extending to the base of the specimen, there is suppurative and granulomatous inflammation with central necrosis.
Diagnosis.—Mycobacterium marinum infection.
Comment
Swimming-pool granuloma and fish-tank granuloma are names for infections that are caused by Mycobacterium marinum. Originally described after its discovery on saltwater fish in the Philadelphia Aquarium in 1926, the first human skin infection was reported in 1951 and occurred in people who swam in contaminated swimming pools. [1] M. marinum is a nontuberculous, atypical mycobacterium, which is found on plants, soil, and fish in freshwater and saltwater worldwide. [2]
Humans become infected usually after trauma and contact with an aquatic environment. Infection is limited to the skin and usually occurs in healthy individuals, but in immunocompromised patients the infection may disseminate or spread to the subcutis and bone. [2] After 2-3 weeks of incubation, the lesions usually appear as solitary nodules or plaques that may lead to suppurative ulcers. Occasionally, there may be sporotrichoid spread along lymphatics. [2]
The differential diagnosis includes sporotrichosis, leishmania, other mycobacterial and deep fungal infections, tularemia, sarcoidosis, and foreign-body reactions. [1]
Histopathologic features of M. marinum infection may include caseating or non-caseating granulomas in the dermis with lymphocytes and macrophages in the infiltrate. Epidermal changes such as ulcers and acanthosis can be seen as well as subcutaneous involvement in some specimens. [2, 3] The organism can be cultured on Lowenstein-Jensen media at 33 C or identified with Ziehl-Neelsen or Fite stains for acid-fast bacilli. [3] Molecular diagnosis makes possible the identification of species of mycobacteria through polymerase chain reaction-restriction analysis length polymorphism of the hsp65 gene. [4] This test provides rapid identification of the cause of the infection, but it does not provide information regarding the susceptibility of the organism to antibiotics.
Treatment options include antibiotic regimens that depend on clinical response. Antibiotics include minocycline 100 mg twice daily, trimethoprim-sulfamethoxazole 160/800 mg twice daily, rifampin 600 mg twice daily, and clarithromycin 500 mg twice daily. A combination course of rifampin-ethambutol was reported as well as use of local heat in conjunction with antibiotics. [2, 5] Other options include surgical debridement and excision.
References
1. Ang P, et al. Retrospective study of Mycobacterium marinum skin infections. Int J Dermatol 2000; 39:343.2. Palenque E, Skin disease and nontuberculous atypical mycobacteria. Int J Dermatol 2000; 39:659.
3. Cosma CL, et al. The secret lives of the pathogenic mycobacteria. Ann Rev Microbiol 2003; 57:641.
4. Pasquale E, et al. Rapid identification of cutaneous infections by nontubecular mycobacteria by polymerase chain reaction-restriction analysis length polymorphism of the hsp65 gene. Int J Dermatol 2001; 40:495.
5. Hisamichi K, et al. Efficacy of oral minocycline and hyperthermic treatment in a case of atypical mycobacterial skin infection by Mycobacterium marinum. J Dermatol 2002; 29:810.
© 2004 Dermatology Online Journal

