Multiple nodular lesions of upper limbs: Nodular mastocytosis
Published Web Location
https://doi.org/10.5070/D38dn6200gMain Content
Multiple nodular lesions of upper limbs: Nodular mastocytosis
Samy Fenniche1, Hayet Marrak1, Mohamed Zghal1, Olfa Khayat2, Achraf Debbiche2, Mohamed Ben Ayed2, Insaf Mokhtar1
Dermatology Online Journal 8(2): 20
1. Dermatology Department. Habib Thameur Hospital. Tunis - Tunisia 2. Histopathology Department. Habib Thameur Hospital. Tunis
- TunisiaCase report
 |
| Figure 1 |
|---|
| Figure 1 : Erythematous pigmented nodules of forearms |
A 14-year-old girl presented with a 3-month history of multiple upper extremity nodules. Physical examination revealed multiple erythematous pigmented nodules, 0.5 to 1 cm in diameter, slightly pruritic, involving the upper limbs (Figure 1). A skin biopsy of a nodular lesion was performed (Figure 2).
 |  |
| Figure 2 | Figure 3 |
|---|---|
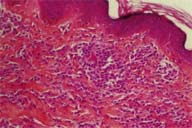
| Figure 2(HES x 20): Mononuclear cell infiltrate of reticular dermis | |
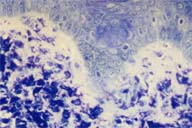
| Figure 3 (toluidine blue stain x 40): Mast cell dermal infiltrate with specific granulations | |
Histopathologic findings
Hematoxylin-eosin staining of the biopsy specimen showed a moderate perivascular mononuclear cell infiltrate in the dermis. Toluidine blue stain revealed the infiltrate to be mainly composed of mast cells with specific metachromatic intracytoplasmic granulations (Figure 3). The diagnosis of cutaneous mastocytosis was made.
Discussion
Mastocytosis results from tissue infiltration by mast cells. It's a rare affliction which may occur at any age, but is mainly seen in infancy. [1] In 65%, the first manifestations appear between birth and 15 years of age. [2] Different clinical forms have been described and the classification mainly depends upon the sites involved and the significance of the involvement. A classification into 5 groups (Table I) was recently proposed. [3]
Cutaneous mastocytosis
(at least one internal organ, with or without skin involvement )
(with or without skin involvement)
(with or without skin involvement) Leukemic mastocytosis |
The clinical forms commonly seen in childhood are urticaria pigmentosa (UP), mastocytoma, and diffuse cutaneous mastocytosis, which is much rarer. [4, 5] UP exhibits a monomorphic macular and papular eruption that is usually erythematous or red-brown. The lesions may be few to very numerous with a "leopard skin-like" presentation. When the clinical lesions are nodular and numerous, such as in our patient, the term UP is not really representative. We agree with one author's proposal to reclassify UP into cutaneous mastocytosis with numerous macules, papules or small nodules. [6]. The predominant sites of lesions are the trunk and the limbs. Urtication at the slightest trauma (Darier's sign) is characteristic. Congestive paroxystic manifestations caused by the abrupt release of histamine can also be seen. A variety of symptoms including pruritus, urticaria, anaphylaxis and flushing are typical. These symptoms were not seen in our case. Systemic symptoms may occur spontaneously or may be caused by emotion, heat or ingestion of certain foods and drugs (Table II).
Food
|
Extracutaneous manifestations associated with UP in childhood are rare and mastocytosis generally follows a benign course if feature the cutaneous eruption occurs before 5 years of age. [3] After this age, 15 to 30% can develop systemic manifestations with palpitation, episodes of flushing and gastrointestinal disorders.
The primary goal is to prevent systemic symptoms and patients should avoid all factors causing mast cell degranulation (Table II). The treatment of cutaneous mastocytosis is symptomatic and consists of anti-histamines (H1) to which H2 anti-histamines may be added as needed, especially in the case of digestive troubles. [1,7] Ketotifen and disodium cromoglycate act as inhibitors of mast cell degranulation and are effective for cutaneous, neurologic, and digestive manifestations. [3] Systemic corticosteroid therapy constitutes an alternative in the case of diffuse cutaneous lesions with systemic manifestations. Topical corticoids under occlusion are mainly indicated in mastocytoma, but have been used in generalized UP and reduce secondary hyperpigmentation. PUVA therapy reduces pruritus but caution is urged to prevent early significant histamine release. PUVA is indicated mainly in severe blistering forms. The possibility of a new treatment acting against mast cell proliferation appears interesting. A "stem cell factor" was identified recently and may be important in the pathophysiology of mastocytosis [8].
In conclusion, cutaneous mastocytosis is generally benign in children and UP is the most common clinical form though descriptions of this entity should be expanded to include nodular forms. In childhood, in the absence of clinical symptoms suggesting systemic involvement, detailed laboratory investigations are not recommended.
References
1. Longley J, Duffy TP, Khon S. The mast cell and mast cell disease. J Am Acad Dermatol, 1995; 32: 546-5612. Azana JM, Torreio A, Mediero IG, Zambrano A. Urticaria pigmentosa. A review of 67 pediatric cases. Pediatr Dermatol, 1994; 11: 102-6
3. Golkar L, Bernard JD. Mastocytosis. Lancet, 1997; 349: 1379-1381
4. Kettelhut BV, Metcalfe DD. Pediatric mastocytosis. J Invest Dermatol, 1991; 96: 15s-18s
5. Legrain V, Taieb A, Bioulac-Sage P, Maleville J. Mastocytose cutanee diffuse sans lesion permanente. Ann Dermatol Venereol, 1994; 121: 561- 64
6. Loubeyres S, Leaute-Labreze C, Roul S, Labbe L, Bioulac-Sage P, Taieb A. Classification et prise en charge des mastocytoses de l'enfant. Ann Dermatol Venereol 1999 ; 126 : 20-25
7. Metcalfe DD. The treatment of mastocytosis: An overview. J Invest Dermatol, 1991; 96: 55s-9s
8. Hamann K, Haas N, Grabbe J, Czarnetzki BM. Expression of stem cell factor in cutaneous mastocytosis. Br J Dermatol, 1995; 133: 203-8
© 2002 Dermatology Online Journal

