Conradi-Hünermann-Happle syndrome
Published Web Location
https://doi.org/10.5070/D38c0053h9Main Content
Conradi-Hünermann-Happle syndrome
Rachael D Hartman MD, Vered Molho-Pessach MD, Julie V Schaffer MD
Dermatology Online Journal 16 (11): 4
Department of Dermatology, New York University, New York, New YorkAbstract
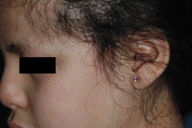
A seven-year-old girl was born with red, scaly skin that later evolved into hypopigmentation and follicular atrophoderma in a widespread distribution that followed Blaschko lines. She also had patchy, scarring alopecia, left microphthalmia, bilateral cataracts, dysmorphic facies, short stature, hip dysplasia, and vertebral abnormalities. An elevated plasma 8(9)-cholestenol level confirmed the diagnosis of Conradi-Hünermann-Happle syndrome, which is caused by mutations in the emopamil binding protein (EBP) gene. This reports highlights the evolution of clinical findings over time in this X-linked dominant form of chondrodysplasia punctata.
History
 |  |
| Figure 1 | Figure 2 |
|---|
 |
| Figure 3 |
|---|
This seven-year-old girl of Mexican descent presented to the Pediatric Dermatology Clinic at the Charles C. Harris Skin and Cancer Pavilion in February, 2009, for evaluation of dry skin and pruritus. She was born with red, scaly skin that persisted until approximately one year of age, when the erythema was replaced by pigmentary alteration. Patchy alopecia was noted at age two years. During early infancy, a diagnosis of left microphthalmia and bilateral cataracts was made. She was found to have scoliosis at age two years and a gait abnormality became evident at age three years. Radiologic evaluation showed normal femoral epiphyses (at age four years), developmental dysplasia of the hips, and spina bifida occulta at L5. She also had C1-C2 stenosis, which was treated with posterior decompression surgery. The patient’s development was mildly delayed and she received physical, occupational, and speech therapy. Her six older siblings were healthy and there was no family history of cutaneous, ocular, or skeletal disease.
Management of the patient’s dry, scaly skin has included daily application of ammonium lactate 12 percent cream, ceramide-enriched emollients, and petrolatum ointment. Intermittent flares of eczematous dermatitis have been treated with various topical glucocorticoids.
Physical examination
The patient was small for her age and had a dysmorphic facial appearance, which included frontal bossing and maxillary hypoplasia. In a widespread distribution that followed Blaschko lines on the chest, back, abdomen, and extremities were hypopigmented streaks and swirls, which were associated with subtle cribriform atrophy and, in some areas, obvious follicular atrophoderma. Adherent, polygonal, brown scales were present on the lower legs. Patchy areas of scarring alopecia of the scalp, eyebrows (especially laterally), and eyelashes were evident.
Laboratory data
Plasma sterol analysis demonstrated elevated levels of 8(9)-cholestenol. The patient’s insurance would not pay for emopamil binding protein (EBP) gene sequencing.
Histopathology
None
Comment
Conradi-Hünermann-Happle syndrome (CHHS) is an X-linked dominant disorder that has cutaneous, skeletal, and ocular manifestations; it also is referred to as X-linked dominant chondrodysplasia punctata [1]. Patients with CHHS are born with ichthyosiform erythroderma that is characterized by feathery, adherent scale and a distribution along Blaschko lines. Histopathologic evaluation typically demonstrates thick, laminated orthokeratosis and keratotic follicular plugs that contain dystrophic calcification [2]. The erythroderma usually resolves spontaneously during the first year of life. Subsequently, residual streaks and swirls of follicular atrophoderma and, occasionally, hyper- or hypopigmentation are evident. Scalp involvement results in patchy, scarring alopecia. Skeletal abnormalities include short stature, craniofacial anomalies (e.g., frontal bossing, malar hypoplasia, and a flat nasal bridge), asymmetric limb reduction defects, vertebral malformations, hip dysplasia, and chondrodysplasia punctata (stippled calcifications of the epiphyses) [1]. The latter often disappears during infancy, which explains our patient’s normal-appearing epiphyses in radiographs taken at four years of age. Ocular anomalies include cataracts, microphthalmia, microcornea, glaucoma, and atrophy of the retina and optic nerve [1].
CHHS is caused by mutations in the emopamil binding protein (EBP) gene, which is located on the short arm of the X chromosome [3]. EBP functions as a Δ8-Δ7-sterol isomerase in the cholesterol biosynthesis pathway, and it catalyzes the conversion of 8(9)-cholestenol to lathosterol. The EBP deficiency that underlies CHHS results in accumulation of 8-dehydrocholesterol and 8(9)-cholestenol in the plasma, skin, and other tissues [3].
Most patients with CHHS are girls with a heterozygous EBP mutation. The Blaschkolinear distribution of skin manifestations reflects the functional mosaicism that occurs in females as a result of lyonization. Mosaicism is also evident in the asymmetric extracutaneous findings of CHHS. For example, the cataracts show a sectorial arrangement that is a likely result of mosaicism [4]. The EBP mutations that underlie CHHS are lethal in male fetuses because of their hemizygous state, but affected boys with Klinefelter syndrome (XXY; also functional mosaics with respect to the X chromosome) or mosaicism caused by an early postzygotic mutation in the EBP gene have been reported [5, 6].
References
1. Happle R. X-linked dominant chondrodysplasia punctata. Hum Genet 1979; 53: 65 [PubMed]2. Hoang MP, et al. Ichthyosis and keratotic follicular plugs containing dystrophic calcification in newborns: distinctive histopathologic features of X-linked dominant chondrodysplasia punctata (Conradi-Hünermann-Happle syndrome). Am J Dermatopathol 2004; 26: 53 [PubMed]
3. Braverman N, et al. Mutations in the gene encoding 3 beta-hydroxysteroid-delta 8, delta 7-isomerase cause X-linked dominant Conradi-Hunermann syndrome. Nat Genet 1999; 22: 291 [PubMed]
4. Happle R. X-chromosome inactivation: role in skin disease expression. Acta Paediatr 2006; 95: 16 [PubMed]
5. Sutphen R, et al. XXY male with X-linked dominant chondrodysplasia punctata (Happle syndrome). Am J Med Genet 1995; 57: 489 [PubMed]
6. Aughton DJ, et al. X-linked dominant chondrodysplasia punctata (CDPX2) caused by single-gene mosaicism in a male. Am J Med Genet 2003; 166A: 255 [PubMed]
© 2010 Dermatology Online Journal

