Calcinosis cutis complicating liver transplantation
Published Web Location
https://doi.org/10.5070/D38bf9j333Main Content
Calcinosis cutis complicating liver transplantation
Amir Houshang Ehsani MD, Robabeh Abedini MD, Maryam Ghiasi MD, Mahbubeh Sadat Hoseini MD
Dermatology Online Journal 12 (7): 23
Tehran University of Medical Sciences, Department of Dermatology, Razi Hospital, Tehran, Iran. mghiasi@razi.tums.ac.ir
Abstract
We report a case of calcinosis cutis in a 41-year-old man developing after liver transplantation at sites where no intravenous calcium had been administered. The cutaneous lesions developed on his right upper arm 10-days post-transplantation. The patient had received calcium chloride solution intravenously after surgery. We excluded other causes of ectopic calcification such as hyperparathyroidism, renal failure, and extravasation of calcium chloride.
Ectopic calcification following liver transplantation has been reported to occur in various internal organs but there have been few reports of skin involvement. The pathogenesis is uncertain with previous reports suggesting that the calcification could be either dystrophic or metastatic. The large amount of intravenous calcium needed to correct hypocalcemia secondary to blood-product transfusion is thought to play a central role. Our case supports an earlier hypothesis that short-lived and often undetected elevations in the calcium-phosphate product may be responsible [1, 2].
Clinical synopsis
A 41-year-old man developed erythematous papules on his right upper arm 10 days after he underwent liver transplantation. The transplant had been for chronic viral hepatitis (hepatitis B). His operation lasted over 8 hours, and intra-operatively he required transfusion of 7 units of packed red cells and 5 units of fresh-frozen plasma. In addition he received 5 units of platelets after surgery. In the immediate post-operative period his immunosuppression consisted of prednisolone, cyclophosphamide, mycophenolate mofetil, and intravenous immunoglobulin.
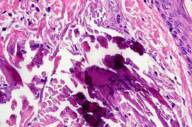
On examination 20-days post-operation he had multiple erythematous hard papules in linear configuration on the extensor aspect of his right upper arm. Within the lesion there were several 1-2 mm white calcifications. No intravenous infusions had been administered in his right upper arm and all intravenous calcium was infused via a central line. Serum levels of calcium, phosphate, and parathyroid hormone remained within normal limits during and after surgery. Renal function was normal throughout this period. On the first 3 days after surgery he received calcium chloride solution intravenously, which was changed to oral calcium carbonate for the next 4 days, and then discontinued. A skin biopsy of the plaque showed a normal epidermis with deposits of calcium within dermal collagen fiber in the reticular dermis. Over the next 4 months the plaque improved partially with some atrophic scarring.
Discussion
Cutaneous calcification or calcinosis cutis may be divided into three main types: dystrophic, metastatic, and idiopathic. In dystrophic calcification, calcium deposits occur in areas of damaged skin in the absence of systemic metabolic abnormalities in calcium regulation. Metastatic calcification occurs in normal tissue when there is a disturbance in systemic calcium homeostasis, as is most commonly encountered in chronic renal failure. The main determinant of metastatic calcification is the solubility product of calcium and phosphate [3].
Few cases have been reported of cutaneous calcification following liver transplantation until now. Munoz et al. observed ectopic soft-tissue calcification in seven patients following liver transplantation. The organs affected, in order of frequency, were the lungs, liver graft, colon, vascular walls, kidneys, adrenal glands, and gastric mucosa. Patients with ectopic calcification received more blood and calcium compared to those with no calcification. However, their serum calcium and phosphate levels remained within or below normal limits [4]. A postmortem study by Wachtel et al. on 25 patients who had undergone liver transplantation found microscopic foci of calcification in various organs in 84 percent of patients; the skin was involved in two cases [5]. Jucgla et al. reported four adults who developed calcinosis cutis 10-21 days after transplantation. In all four cases the calcification occurred on the upper limbs at sites where intravenous calcium had been infused. None of the patients had documented hypercalcemia or hyperphosphatemia, and parathyroid hormone levels and renal function were normal. The lesions improved or resolved within the next 2-6 months in the three patients who were followed [6]. Larralde et al. reported cutaneous calcification on the trunk in a 3-year-old girl 10 days following liver transplantation. No hypercalcemia, hyperphosphatemia or renal failure was recorded [7]. More recently another case of calcinosis cutis was reported in a 22-year-old woman by Lateo et al. She developed a calcified plaque on her upper arm one month after liver transplantation. The patient had no elevation in serum calcium, phosphate, or parathyroid hormone, and no disturbance in renal function [3]. As in our case, in these recent reports the cutaneous calcification did not occur at a calcium infusion sites and the patients had received large amounts of blood-product transfusion and intravenous calcium.
It has been suggested that the pathogenesis of ectopic calcification following liver transplantation is multifactorial [4]. During liver transplantation, hypocalcemia develops as result of calcium chelating with citrate from transfused blood products, particularly during the anhepatic phase when citrate accumulates owing to absence of hepatic metabolism. This necessitates routine use of intravenous calcium supplementation during liver transplantation [3]. We suggest in our patient the calcification was the metastatic type. It is possible that transient and undetectable elevations of calcium levels occur when intravenous calcium is administered; this could result in short-lived periods during which the calcium-phosphate solubility product is elevated, resulting in metastatic calcification. Frequent monitoring of serum calcium and phosphate levels in the early post-operative period, particularly in patients who have received large amounts of blood product, could help to identify elevations in calcium-phosphate product at an early stage. Prompt treatment to reduce the calcium-phosphate product may help to prevent this complication.
References
1. Walsh JS, Fairley JA. Calcifying disorders of the skin. J Am Acad Dermatol 1995 Nov; 33(5 pt 1): 693-706. PubMed2. Touart DM, Sau P. Cutaneous deposition diseases. Part II. J Am Acad Dermatol. 1998 Aug; 39(2 Pt 1):149-71; quiz 172-4. Review. Erratum in: J Am Acad Dermatol 1998 Dec; 39(6):1042. PubMed
3. Lateo S, Charlton F, Hudsont M, Lawrence CM. Cutaneous calcification following liver transplantation. Clin Exp Dermatol 2005 Sep; 30(5): 484-6. PubMed
4. Munoz SJ, Nagelberg SB, Green PJ, Angstadt JD, Yang SL, Jarrell BE, Maddrey WC. Ectopic soft tissue calcium deposition following liver transplantation. Hepathology 1998 May-Jun; 8(3): 476-83. PubMed
5. Wachtel MS, Khettry U, Arkin CF. Tissue calcification after orthotopic liver transplantation. An autopsy study. Arch Pathol Lab Med. 1992 Sep; 116(9):930-3. PubMed
6. Jucgla A, Sais G, Curco N, Marcoval J, Moreno A, Peyri J. Calcinosis cutis following liver transplantation: a complication of intravenous calcium administration.Br J Dermatol. 1995 Feb; 132(2):275-8. PubMed
7. Larralde M, Giachetti A, Kowalczuk A, D' Agostino D, Galimberti R. alcinosis cutis following liver transplantation in a pediatric patient. Pediatr Dermatol. 2003 May-Jun; 20(3):225-8. PubMed
© 2006 Dermatology Online Journal