Pairing and comparing nine diseases with Degos Disease (Malignant Atrophic Papulosis): An attempt to illustrate our understanding and direct future inquiry
Published Web Location
https://doi.org/10.5070/D381n2q8zdMain Content
Pairing and comparing nine diseases with Degos Disease (Malignant Atrophic Papulosis): An attempt to illustrate our understanding
and direct future inquiry
Noah Scheinfeld MD JD
Dermatology Online Journal 15 (1): 10
Department of Dermatology, Columbia University, New York, NY. NSS32@columbia.eduAbstract
Degos disease is a poorly defined condition that encompasses cutaneous and systemic findings that overlap with a large number of other rheumatologic and coagulation disorders. Comparisons are made herein with 9 conditions that share findings and presentations.
A version of this paper was delivered at the American College of Rheumatology (ACR) Study Group on Degos Disease, Thromboangiitis Obliterans, and Related Vasculopathies on November 9, 2007 under the title "Parallel Diseases and Degos Pathophysiology." [1]
Introduction
Degos disease is an extremely rare and poorly understood disease. This paper seeks to cast some light on Degos disease by comparing its cutaneous manifestations to those seen in nine other entities that share similar findings and presentations. Diseases, disease states, and disease findings that will be compared to Degos include: (1) diseases with cutaneous and systemic variants, (2) white atrophic diseases that occur on the penis, (3) generalized non-infectious eruptions with disseminated coagulopathies, (4) white atrophic skin diseases with or without coagulopathies, (5) generalized eruptions of round ulcerated nodules, (6) collagen vascular diseases in which manifestations include Degos-type white atrophic papules, (7) skin diseases with dermal mucin, (8) skin diseases with interface dermatitis, and (9) genetic diseases including familial Degos disease. (Table 1)
Characteristics of Degos Disease
In order to compare findings with other diseases we must first discuss and define Degos Disease in brief. This is done in Table 2 [2].
I. Skin diseases with cutaneous and systemic variants
Several diseases, including Degos, have variants that are confined to the skin and systemic variants that exhibit cutaneous and internal involvement. (Table 4). It is poorly understood what mechanisms determine cutaneous or single organ limitations versus systemic extensions of disease.
Table 3 Pairings Ia
Table 4 Pairings Ib
 |  |
| Figure 1a | Figure 1b |
|---|---|
| Figures 1a & 1b. 1a. Localized Degos 1b. Systemic Degos (skin, gastrointestinal, and neurological involvement) | |
 |  |
| Figure 2a | Figure 2b |
|---|---|
| Figures 2a & 2b: 2a. Discoid Lupus Erythematosus 2b. Systemic Lupus Erythematosus | |
 |  |
| Figure 3a | Figure 3b |
|---|---|
| Figures 3a & 3b. 3a. Morphea 3b. Systemic Sclerosis | |
 |  |
| Figure 4a | Figure 4b |
|---|---|
| Figures 4a & 4b. 4a. Local Sarcoid 4b. Sarcoid occurring with bilateral lyphmadentopathy | |
 |  |
| Figure 5a | Figure 5b |
|---|---|
| Figures 5a & 5b. 5a. Psoriasis Vulgaris 5b. Psoriatic Arthritis | |
 |  |
| Figure 5c | Figure 5d |
|---|---|
| Figures 5c & 5d. 5c. Hidradenitis 5d. Hidradenitis in patient with spondylarthropathy and pilonidal cyst | |
II. White atrophic diseases that occur on the penis
Degos disease manifests with white and purple atrophic, sometimes crusted, papules on the penis. Another disease that can manifest similarly is lichen sclerosis (LS) Table 5 Pairings II.
Degos disease and lichen sclerosis are seldom lumped together, but perhaps they should be. Harvell [4] described the histology in a case of Degos disease and found that it resembled that of lichen sclerosis. Specifically the features Harvell noted were:
- Fully developed papules were raised, umbilicated with porcelain-white centers and surrounding red rims.
- Histology showed prominent interface reaction with squamatization of the dermo-epidermal junction, melanin incontinence, and epidermal atrophy.
- A developing zone of papillary dermal sclerosis resembled the early stages of lichen sclerosus et atrophicus in miniature.
It is unclear why LS and forms of Degos disease manifest on the penis. Whereas the skin looks like a single organ, site differences impact function and disease in ways for which we have yet to account.
III. Generalized non-infectious eruptions with disseminated coagulopathies
The most basic pathologic element of Degos disease is a vasculopathy/endovasculitis associated with pathologic coagulation. Antiphospholipid syndrome is also a disease marked by pathologic coagulation. However, these disease have totally different cutaneous manifestations (Table 6). Some manifestations of vasculopathies can be explained simply by the size of the vessel involved, but many other manifestations elude explanation. As a result Degos and antiphospholipid syndrome or livedo reticularis clinically manifest in wholly dissimilar fashion.
Table 5 Pairings II
 |  |
| Figure 7a | Figure 7b |
|---|---|
| Figures 7a & 7b. 7a. Digital Necrosis of severe antiphospholipid syndrome 7b. Focal necrosis of Degos papule | |
 |  |
| Figure 7c | Figure 7d |
|---|---|
| Figures 7c & 7d. 7c. Bland reticular Pattern of livedo reticularis 7d. Bland white atropic papule of Degos | |
IV. White atrophic skin diseases (with coagulopathy highlighted in yellow)
Degos disease often exhibits white atrophic skin associated with coagulopathy. Atrophie blanche (AB), (also termed livedoid vasculopathy), is another disease associated with coagulopathy that manifests with white atropic plaques. (Table 7) [lichen sclerosus is included in this table because it resembles both Degos and atrophie blanche]. Protein deficiencies (C and S), Factor V Leiden and several pathologic states that lead to hypercoagulation are associated with atrophie blanche. Degos disease is not associated with atrophie blanche. Hairston [6] reviewed the tertiary care records of 45 patients with biopsy-proven livedoid vasculopathy. He found that 32 (71.1%) were female with a mean age of 45 years (10-85). Additional findings included:
- Bilateral lower extremity disease occurred in 36 patients (80.0%), ulceration in 31 (68.9%), and atrophie blanche in 32 (71.1%).
- In patients tested, transcutaneous oximetry measurements were decreased in 20 (74.1%) of 27,
- Factor V Leiden mutation (heterozygous) was noted in 2 (22.2%) of 9, decreased activity for protein C or protein S in 2 (13.3%) of 15, prothrombin G20210A gene mutation in 1 (8.3%) of 12, and lupus anticoagulant in 5 (17.9%) of 28.
- Anticardiolipin antibodies were present in 8 (28.6%) of 28 patients and elevated homocysteine levels in 3 (14.3%) of 21.
- Intraluminal thrombosis was seen in 44 (97.8%) of 45 skin biopsy specimens.
- Direct immunofluorescence disclosed multiple vascular conjugates in 31 (86.1%) of 36 biopsy specimens.
Table 7 Pairings IV
It is interesting that Degos disease lacks the identification of a measurable pathologic factor or deficiency as is found in several other coagulopathies, particularly ones associated with atrophie blanche. Occlusion can be effected at several steps involving blood flow, coagulation pathway steps and vessel size.
 |  |
| Figure 8a | Figure 8b |
|---|---|
| Figures 8a & 8b. 8a. Degos round/oval papules 8b. Atrophie blanche-stellate atrophic plaque on leg | |
 |
| Figure 8c |
|---|
| Figure 8c. LSA on the breast some what polymorphous in shape |
V. Round ulcerated generalized nodules
The original index case of Degos disease is considered to be that of Kohlmeier published in 1941 [7]. Although he called his case thromboagiitis obliterans, his patient is now considered to be a case of Degos Disease. When I look at these pictures now, I think of another disease of nodules with central crusting-lymphomatoid papulosis (Table 8 Pairings V). Whereas Kohlmeier's case looks like lymphomatoid papulosis it is not!
 |
| Figure 9a |
|---|
| Figures 9a & 9b. Kohlmeier's initial photographs of what we now call Degos Disease published in 1941 |
Why should Degos disease and lymphomatoid papulosis look alike? We do not know fully why the contours of various eruptions are round, ovate or irregular. What factors lead to involvement or sparing? We still need to define why the eruption of Degos is round or oval. If we understood this we might have more insights into the pathogenesis of Degos disease.
 |  |
| Figure 9c | Figure 9d |
|---|---|
| Figure 9c. Generalized crusted papules of lymphomatoid papulosis Figure 9d. Generalized crusted papules of Degos | |
VI. Collagen Vascular Diseases manifesting with Degos-like papules
Degos disease is sometimes categorized with Collagen vascular diseases (CVD). Evidence used to buttress this argument comes from the fact that some rare cases of CVD manifest with Degos-like white atropic papules and various types of vascular occlusion (Table 9 Pairings VI).
I have argued that [8] Degos disease differs from lupus erythematosus in a number of ways. Degos disease is characterized by:
1. Unresponsiveness to therapy;
2. Frequent presence of cellular virus-like inclusions;
3. Negative DIF findings;
4. Invariably fatal course usually in 1 to 3 years from diagnosis;
5. Lack of photosensitivity;
6. Lack of facial lesions.
7. White atrophic papules whose histology is a sensitive rather than specific indication of DD.
Despite the fact that I think Degos differs from lupus and other collagen vascular diseases (CVD), I find it is unsurprising that complex diseases of dysregulation like CVD have among their incarnations Degos mimics.
VII. Diseases with dermal mucin
Degos is one of the many dermatological diseases that histologically demonstrates mucin (Table 10 Pairings VIII Diseases with Mucin).
Why mucin characterizes these disparate diseases is unclear. The role of mucin in normal function and disease is similarly unclear. The ubiquity of mucin suggests that its function involves many systems.
VIII. Diseases with interface dermatitis
Many diseases are marked by interface dermatitis (i.e., lymphocytes at the dermal epidermal junction). Degos is one of these diseases. The impact of hematologic/clotting systems on lymphocytes may relate to the occurrence of interface dermatitis. Unfortunately the interactions of these systems are poorly understood.
Table 11 Pairings IX Conditions with interface dermatitis
IX. Genetic diseases generally, familial Degos in particular
At least 10 case reports note the existence of familial Degos disease (Table 12). The Online Mendalian Inheritance in Man (OMIM) has given Degos disease a number --#602248. Because no gene has yet been cloned and possible associated groups of genes might simply increase the odds ratio of getting Degos disease, perhaps Degos disease does not deserve an OMIM number. Alternative possible causes could include a virus or an environmental exposure; there is just very little hard evidence.
Table 12 Pairings X Reports of familial Degos
Conclusion
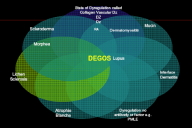 |
| Figure 10 |
|---|
The widely varying manifestations of Degos disease resemble and overlap with many diseases, but still stand apart from the other conditions discussed in this paper (Figure 10). To me, Degos is some type of dysregulation of clotting in which a new pathologic set point for clotting has been established. Thinking of Degos disease as a dysfunctional, but stable set point leading to hypercoagulation explains why therapy is so unsuccessful.
Some day the enigma of Degos will be explained. Currently, the overlap of complex continuously acting systems hides definition of Degos behind a vale of complex effects.
References
1. http://www.degosdisease.com/events/2007_11_09-program.2. Scheinfeld N. Malignant atrophic papulosis. Clin Exp Dermatol. 2007 Sep;32(5):483-7. [PubMed]
3. Lowney ED, Simons HM. "Rheumatoid" nodules of the skin: their significance as an isolated finding. Arch Dermatol 1963; 88:853-8. [PubMed]
4. Harvell JD, Williford PL, White WL. Benign cutaneous Degos' disease: a case report with emphasis on histopathology as papules chronologically evolve. Am J Dermatopathol. 2001 Apr;23(2):116-23. [PubMed]
5. Diógenes MJ, Diógenes PC, de Morais Carneiro RM, Neto CC, Duarte FB, Holanda RR. Cutaneous manifestations associated with antiphospholipid antibodies. Int J Dermatol. 2004 Sep;43(9):632-7. [PubMed]
6. Hairston BR, Davis MD, Pittelkow MR, Ahmed I. Livedoid vasculopathy: further evidence for procoagulant pathogenesis. Arch Dermatol. 2006 Nov;142(11):1413-8. [PubMed]
7. Kohlmeier W. Multiple Hautnelnosen bei Thromboangiitis obliterans. Arch Dermatol Syphilol 1941; 181: 783-4.
8. Scheinfeld N. Degos' disease is probably a distinct entity: a review of clinical & laboratory evidence. J Am Acad Dermatol. 2005;52(2):375-6; author reply 376-8. [PubMed]
© 2009 Dermatology Online Journal



