Burkitt lymphoma with cutaneous involvement
Published Web Location
https://doi.org/10.5070/D37ss667dzMain Content
Burkitt lymphoma with cutaneous involvement
David R Berk MD1, Amy Cheng MD1, Anne C Lind MD2, Susan J Bayliss MD1
Dermatology Online Journal 14 (2): 14
1. Department of Internal Medicine and Pediatrics, Division of Dermatology, Washington University School of Medicine and St.
Louis Children's Hospital, St. Louis, MO. DBerk@im.wustl.edu 2. Department of Pathology and Immunology (AL), Washington University School of Medicine and St. Louis Children's Hospital, St. Louis, MO
Clinical synopsis
A 25-year-old HIV-infected man, on highly active antiretroviral therapy with CD4 count of 198 cells/mμL and viral load of 13,800 copies/mL, presented with a 2-month history of progressive, painful left axillary lymphadenopathy, which was 11 cm. Lymph node biopsy revealed a malignant lymphoid population of cells with intermediate size, mature chromatin, several small eccentrically located nucleoli, a high mitotic rate, and a clonal CD19+, CD20+, CD10+ B-cell immunophenotype. There was effacement of lymph node architecture, necrosis, and many tangible-body macrophages imparting a starry-sky appearance. Burkitt lymphoma was diagnosed. Peripheral blood, cerebrospinal fluid, and bone marrow biopsy were negative for leukemic cells. Clinically and radiographically, the lymphoma increased in size over the next 10 months, extending to overlying muscle and skin, despite receiving 3 cycles of fractionated cyclophosphamide, vincristine, adriamycin, and dexamethasone, palliative radiation therapy, 4 cycles of rituximab, ifosfamide, carboplatin, and etoposide, and prophylactic intrathecal methotrexate.
Approximately 10 months after being diagnosed with Burkitt lymphoma, he was referred to the dermatology service with a 2-month history of an enlarging, erosive plaque over his left axilla, chest, and abdomen. A computed tomography (CT) 1 month earlier had revealed multiple large, enhancing, necrotic, soft tissue masses involving the left axilla, chest, and abdomen, with overlying skin thickening and nodularity, as well as an exo-enteric, ulcerating gastric fundus mass. The radiology service interpreted the masses as Burkitt lymphoma although infection could not be excluded. The oncologists treated him empirically for cellulitis, but wound and blood cultures were negative and he did not respond to antibiotics.
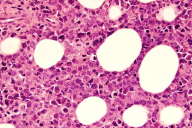
Physical examination revealed a large, erythematous, slightly indurated, centrally verrucous plaque along the left chest wall and abdomen with erosions and bullae (Fig. 1). The remaining physical examination was normal. Skin biopsy from the abdomen revealed full-thickness abnormalities. The epidermis was acanthotic and spongiotic with scattered dyskeratotic keratinocytes. There was prominent extravasation of erythrocytes and an infiltrate filling the dermis and the sampled subcutis (Fig. 2), composed of mononuclear cells with minimal cytoplasm, multiple small nucleoli, and abundant apoptotic forms, consistent with cutaneous Burkitt lymphoma. Repeat CT at the time of skin biopsy demonstrated an interval increase in the left axillary mass which extended down to the iliac crest, and infiltrated the left pectoralis major, deltoid, subscapularis, serratus anterior, and left external oblique muscles. He was treated with nelarabine and high-dose methotrexate but expired 6 weeks later from progressive disease and sepsis from Candida albicans.
Discussion
Burkitt lymphoma is an aggressive non-Hodgkin lymphoma which can be classified into endemic, sporadic, and immunodeficiency variants [1]. Although each variant frequently involves extranodal sites, cutaneous involvement with Burkitt lymphoma is very rare [2, 3, 4, 5, 6, 7]. In most lymphomas and leukemias, cutaneous involvement occurs through hematogenous dissemination. However, cases of cutaneous Burkitt lymphoma have typically resulted from tumor seeding after surgical procedures[4] or local invasion of rapidly enlarging underlying tumors [2, 3]. In our case, cutaneous involvement likely resulted from the former, in the context of widespread multiorgan disease. Our patient's cutaneous Burkitt lymphoma was initially misdiagnosed as cellulitis. Persistent skin lesions in patients with Burkitt lymphoma, especially in proximity to known tumor foci, should raise concern for cutaneous Burkitt lymphoma.
References
1. Blum KA, Lozanski G, Byrd JC. Adult Burkitt leukemia and lymphoma. Blood. Nov 15 2004;104(10):3009-3020. PubMed2. Jacobson MA, Hutcheson AC, Hurray DH, Metcalf JS, Thiers BH. Cutaneous involvement by Burkitt lymphoma. J Am Acad Dermatol. Jun 2006;54(6):1111-1113. PubMed
3. Bachmeyer C, Bazarbachi A, Rio B, et al. Specific cutaneous involvement indicating relapse of Burkitt's lymphoma. Am J Hematol. Feb 1997;54(2):176. PubMed
4. Aractingi S, Marolleau JP, Daniel MT, Brice P, Gisselbrecht C. Subcutaneous localizations of Burkitt lymphoma after celioscopy. Am J Hematol. Apr 1993;42(4):408. PubMed
5. Busschots AM, Geerts ML, Mecucci C, Stul M, Cassiman JJ, van den Berghe H. A translocation (8;14) in a cutaneous large B-cell lymphoma. Am J Clin Pathol. May 1993;99(5):615-621. PubMed
6. Banks PM, Arseneau JC, Gralnick HR, Canellos GP, DeVita VT, Jr., Berard CW. American Burkitt's lymphoma: a clinicopathologic study of 30 cases. II. Pathologic correlations. Am J Med. Mar 1975;58(3):322-329. PubMed
7. Evans HL, Winkelmann RK, Banks PM. Differential diagnosis of malignant and benign cutaneous lymphoid infiltrates: a study of 57 cases in which malignant lymphoma had been diagnosed or suspected in the skin. Cancer. Aug 1979;44(2):699-717. PubMed
© 2008 Dermatology Online Journal