Langerhans cell histiocytosis of vulva
Published Web Location
https://doi.org/10.5070/D37s44j1kfMain Content
Langerhans cell histiocytosis of vulva
Angel Fernandez Flores MD PhD1, Susana Mallo MD2
Dermatology Online Journal 12 (1): 15
Services of Histopathology1 and Dermatology2, Hospital el Bierzo, Ponferrada-Leon, Spain. gpyauflowerlion@terra.esAbstract
Cutaneous involvement of the vulva by Langerhans cell histiocytosis in women older than 70 is a rare phenomenon. A tendency of the disease to involve genital areas, has been described. We present a case of a 72-year-old woman, who had cutaneous vulvar involvement by Langerhans-cell histiocytosis, diagnosed by biopsy. An immunohistochemical study is also described.
Clinical synopsis
A 72-year-old woman was examined by the dermatologist because of discomfort and a pain in the left groin. Some 24 years before, she underwent hysterectomy and bilateral oophorectomy because of multiple leiomyomas. We were not unable to obtain access to that pathology report.A week before the current complaint, the patient underwent mastectomy and axillary lymphadenectomy for resection of an infiltrative carcinoma of the left breast (G3, pT2, pN3a, pM1). The skin exam revealed the presence of a lineal fissure in the left groin, 6 × 1.5 cm, with papular borders (Fig. 1). Many small papules surrounding this main lesion were present. A similar minor lesion was present in the right groin (Fig. 2).
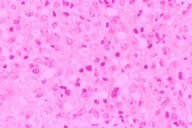
A biopsy of the main lesion was performed, revealing a superficial and deep dermal infiltrate by Langerhans cells (LC) (Fig. 3). These cells showed epidermotropism, infiltrating the dermo-epidermal junction (Fig. 4). In the immunohistochemical study, LC expressed S-100 and CD1a (Fig. 5), but did not express CD34, HMB-45, CD31, or factor VIII. A lymphocyte-rich inflammatory infiltrate was present, composed mainly of CD3(+) T-cells. The infiltrate contained also a moderate number of eosinophils.
 |  |
| Figure 1 | Figure 2 |
|---|---|
| Figure 1. Linear fissure on the left groin. | |
| Figure 2. Lesions on both groins. | |
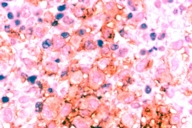 |
| Figure 5 |
|---|
| Figure 5. Expression of CD1a by Langerhans cells. |
The bone gammagraphy showed several hypercaptating lesions in the skull, maxillae, sternum, scapulae, spine, humeri, sacrum, left femur and the right ribs. The abdominal echography showed several hepatic lesions in both lobules, consistent with metastases. Because Ca-15.3 marker in the blood was 228.22 units/ml, the bone as well as the hepatic lesions were interpreted clinically as metastases of breast carcinoma. No biopsies were taken to exclude systemic histiocytosis. The cutaneous lesions were treated with topic corticosteroids, resulting in nearly complete reepithelialization in one month.
Discussion
LC histiocytosis is a disease in which there is pathological LC infiltrate in one or more organs [1]. The disease presents mainly in children, and, when it is seen in adults, it mainly affects the axial skeleton and the skull [2]. Only around 4-7 percent of cases present involvement of the skin as the only organ affected [1, 3], and only around 2 percent of patients with LC histiocytosis, either multisystem or localized, are older than 70 [1].
There is a slight preference for the disease to appear in men [1, 3].
All this makes the combination of "female patient", "older than 70", plus "only skin involvement", quite rare. Only very few examples of these characteristics have been published in literature [4, 5, 6], and mainly in the form of case reports. Even if cases with systemic LC histiocytosis are considered, the cutaneous involvement by the disease is still quite infrequent in women older than 70 years [1, 5, 7].
A predilection for developing LC histiocytosis in anogenital skin has been reported [3, 5, 6, 8, 9, 10, 11, 12, 13, 14, 15]. Some authors speculate that this is related to compromise of the lymph nodes serving the uterine cervix based on immunological response to cervical infection [16, 17] or even a response to smoking [18]. The genital location of LC histiocytosis is especially common in older women, in whom the disease may involve the vulva, extending to the perineum, the perianal area [19], the fourchette, and the clitoris [20]. Clinically, this involvement is seen as scaly papules or sometimes a pruritic rash [5, 21]. Perianal ulceration [19] and vulvar ulcers are rare manifestations of the disease [19, 22]. Systemic involvement is not necessarily present at the same time as the cutaneous disease, but it can appear much later [9].
Prognosis in elderly patients with skin-only involvement is usually good [5]. There is usually a good response to topical treatment, but it is not unusual for the disease to be progressive or recurrent [6]. Good responses are seen with topical nitrogen mustard [5]. Corticoids have played a role in the treatment of LC histiocytosis [7, 9, 23], although they are not always a successful form of treatment [21, 24].
Some have precluded the complete excision of the lesion as a treatment [9]. Other drugs that have been used in the treatment of this disease include vincristine (with very conflicting results) [14, 15], and thalidomide [25, 26]. Although radiotherapy has usually been dismissed as a therapeutic weapon against only-skin involvement by LC histiocytosis, favorable results are sometimes achieved [12,19].
Acknowledgments: We would like to express our gratitude to Dra. Teresa Ribas from Hospital de Leon, thanks to whom, we had the immunohistochemical study for C1a performed.
References
1. Aricò M, Girschikofsky M, Généreau T, Klersy C, McClain K, Grois N, Emile JF, Lukina E, De Juli E, Danesimo C. Langerhans cell histiocytosis in adults: report from the International Registry of the Histiocyte Society. Eur J Cancer. 2003 Nov;39(16):2341-8. PubMed.2. Baumgartner I, von Hochstetter A, Baumert B, Luetolf U, Follath F. Langerhans'-cell histiocytosis in adults. Med Pediatr Oncol. 1997 Jan;28(1):9-14. PubMed.
3. Howarth DM, Gilchrist GS, Mullan BP, Wiseman GA, Edmonson JH, Schomberg PJ. Langerhans cell histiocytosis: diagnosis, natural history, management and outcome. Cancer. 1999 May 15;85(10):2278-90. PubMed.
4. Nethercott JR, Murray AH, Medwidsky W. Histiocytosis X in two adults. Arch Dermatol. 1983 Feb;119(2):157-61. PubMed.
5. Szepietowski J, Toonstra J, Van der Putte SCJ, Tegelberg-Stassen MJAM, Van Vloten WA. Langerhans-cell histiocytosis in a nonagenarian: report of a case with literature review of patients older than 70 years. Eur J Dermatol. 1994; 4(3): 216-220.
6. Axiotis CA, Merino MJ, Duray PH. Langerhans cell histiocytosis of the female genital tract. Cancer. 1991 Mar 15;67(6):1650-60. Review. PubMed.
7. Imanaka A, Tarutani M, Itoh H, Kira M, Itami S. Langerhans cell histiocytosis involving the skin of an elderly woman: a satisfactory remission with oral prednisolone alone. J Dermatol. 2004 Dec;31(12):1023-6. Review. PubMed.
8. Dietrich JE, Edwards C, Laucirica R, Kaufman RH. Langerhans cell histiocytosis of the vulva: two case reports. J Low Genit Tract Dis. 2004 Apr;8(2):147-9. PubMed.
9. Ishigaki H, Hatta N, Yamada M, Orito H, Takehara K. Localised vulva Langerhans cell histiocytosis. Eur J Dermatol. 2004 Nov-Dec;14(6):412-4. Review. PubMed.
10. Meehan SA, Smoller BR. Cutaneous Langerhans cell histiocytosis of the genitalia in the elderly: a report of three cases. J Cutan Pathol. 1998 Aug;25(7):370-4. PubMed.
11. Hoang MP, Owen SA, Haisley-Royster C, Allen MH, Shea CR, Selim MA. Papular eruption of the scalp accompanied by axillary and vulvar ulcerations. Arch Dermatol. 2001;137; 1241-1246.
12. Takata M, Taniguchi A, Imai T, Hirone T, Nonomura A, Fukui Y. An adult case of histiocytosis X with a vulvar ulcer and multiple bone lesions. J Dermatol. 1994 Apr;21(4):259-63. PubMed.
13. Voelklein K, Horny HP, Marzusch K, Dietl J. Primary Langerhans cell histiocytosis of the vulva. Gynecol Obstet Invest. 1993;36(3):189-90. PubMed.
14. Van Savell, Hanna R, Benda J, Argenyi Z. Histiocytosis X of the vulva with a confusing clinical and pathologic presentation: a case report. J Reprod Med. 1995 Apr;40(4):323-6. PubMed.
15. Solano T, España A, Sola J, Lopez G. Langerhans' cell histiocytosis on the vulva. Gynecol Oncol. 2000 Aug;78(2):251-4. Review. PubMed.
16. Morris HHB, Gatter KC, Sykes G, Casemore V, Mason DY. Langerhans' cells in human cervical epithelium: effects of wart virus infection and intraepithelial neoplasia. Br J Obstet Gynaecol. 1983 May;90(5):412-20. PubMed.
17. McArdle JP, Muller HK. Quantitative assessment of Langerhans' cells in human cervical intraepithelial neoplasia and wart virus infection. Am J Obstet Gynecol. 1986 Mar;154(3):509-15. PubMed.
18. Barton SE, Jenkins D, Cuzick J, Maddox PH, Edwards R, Signer A. Effect of cigarette smoking on cervical epithelial immunity: a mechanism for neoplastic change? Lancet. 1988 Sep 17;2(8612):652-4. PubMed.
19. Modi D, Schulz J. Skin ulceration as sole manifestation of Langerhans-cell histiocytosis. Clin Exp Dermatol. 1991 May;16(3):212-5. Review. PubMed.
20. Lichtenwald DJ, Jakubovic HR, Rosenthal D. Primary cutaneous Langerhans cell histiocytosis in an adult. Arch Dermatol. 1991 Oct;127(10):1545-8. PubMed.
21. Smolle J, Kerl H. Cutaneous histiocytosis X in an old patient. In: Wilkinson DS, Mascaro JM, Orfanos CE, editors. Clinical Dermatology (The CMD case collection; World Congress of Dermatology; Berlin (West), May 24-29, 1987, Stuttgard). New York. Schattaver, 1987: 251-252.
22. Rose PG, Johnston GC, Toole RV. Pure cutaneous histiocytosis X of the vulva. Obstetric Gynaecology. 1984;64; 587-591.
23. Wolfson SL, Botero F, Hurwitz S, Pearson HA. "Pure" cutaneous histiocytosis-X. Cancer. 1981;48; 2236-2238.
24. Perrot H, Garnier C, Claudy A, Thivolet J. Histiocytosis X chez un adulte âgé. Bull Soc Fr Derm Syph. 1970;78; 194-195.
25. Misery I, Larbre B, Lyonnet S, Faure M, Thivolet J. Remission of Langerhans cell histiocytosis with thalidomide treatment. Clin Exp Dermatol. 1993;18; 487.
26. Meunier I, Marck Y, Ribeyre C, Meynadier J. Adult cutaneous Langerhans cell histiocytosis: remission with thalidomide treatment. Br J Dermatol. 1995;132; 168.
© 2006 Dermatology Online Journal