Pancreatic panniculitis: A rare form of panniculitis
Published Web Location
https://doi.org/10.5070/D37f08v0w9Main Content
Pancreatic panniculitis: A rare form of panniculitis
NP Madarasingha MD1, K Satgurunathan MD2, Ruchira Fernando MD3
Dermatology Online Journal 15 (3): 17
1. Senior Registrar, Department of Dermatology2. Consultant Dermatologist, Department of Dermatology
3. Consultant Pathologist, Department of Pathology
National Hospital of Sri Lanka, Columbo, Sri Lanka. nayanimadara@yahoo.com
Abstract
Pancreatic panniculitis is rare form of panniculitis with associated pancreatic disease. The skin manifestations can occur at any time of the pancreatic pathology. Here we report a case of pancreatic panniculitis associated with underlying chronic pancreatitis. The patient presented with painful subcutaneous nodules and the histology revealed the characteristic features of pancreatic panniculitis.
Introduction
Pancreatic panniculitis is a rare cutaneous manifestation in patients with underlying pancreatic disease. It is mostly associated with acute or chronic pancreatitis and pancreatic carcinoma, frequently of acinar cell type [1]. Less frequent associations include pseudocyst, vasculopancreatic fistulas and pancreas divisum. The skin manifestation can predate, occur concurrently with, or lag behind the pancreatic pathology [1, 2].
Case History
A 35-year-old male presented with a 4 week history of painful subcutaneous nodules on shins and buttocks. He had loss of weight and loss of appetite. He did not have fever, arthralgia, or chronic cough and his bowel habits were normal. He reported consumption of about half a bottle of hard liquor per day. Three months prior to presentation he had an episode of severe central abdominal pain associated with nausea and vomiting and was diagnosed as having chronic pancreatitis.
Physical examination revealed multiple tender subcutaneous nodules over the ankle region, shins, thighs, and buttocks. The overlying skin was erythematous with no change in skin texture. None of the lesions was ulcerated. Systemic examination was normal except for mild pallor. Clinically, the possibilities of erythema nodosum, erythema induratum, or pancreatic panniculitis were entertained. Whitish oily material was noted when performing the incisional biopsy, favoring fat necrosis.
His erythrocyte sedimentation rate (ESR) was 26 mm; hemoglobin was 9.2 g/dl with normal white cells and platelets and additional testing suggested anemia of chronic disease. Antistreptolysin O titer (ASOT) was <200 IU, chest X-ray was normal, and Mantoux was negative. Serum amylase was elevated to three times the upper limit. His CT scan of the abdomen, done 2 months prior, revealed features of chronic pancreatitis with no evidence of malignancy.
The histology of the skin nodule showed characteristic features of pancreatic panniculitis with mostly lobular panniculitis with inflammatory infiltrate and intense necrosis of the adipocytes.
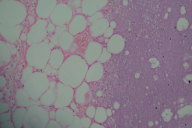 | 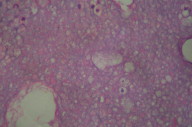 |
| Figure 1 | Figure 2 |
|---|---|
| Figure 1. H&E x10 Figure 2. H&E x40 | |
Discussion
Pancreatic panniculitis is a rare entity appearing in approximately 2-3 percent of all patients with pancreatic disease [1]. Rarely it can manifest in patients with subclinical pancreatic disease or with no pancreatic disease with high serum levels of pancreatic lipase of unknown origin [3]. It has a distinct clinical picture of erythematous tender subcutaneous nodules that spontaneously ulcerate to discharge thick oily material. The usual sites are the distal parts of the lower extremities but involvement of areas such as breasts, buttocks, thighs, and abdomen are described [1]. The onset of the panniculitis is commonly associated with acute arthritis with necrosis of the periarticular fat tissue [1]. Necrosis of the fat at distant foci leading to a fatal outcome is documented rarely [1, 2].
Pancreatic lipase and amylase are known to have a pathogenic role causing subcutaneous fat necrosis. This is supported by the finding of these enzymes in the areas of subcutaneous fat necrosis [3].
Histopathological examination is required for the diagnosis of this entity and shows characteristic features of mostly lobular panniculitis with intense necrosis of adipocytes [4]. These necrotic adipocytes with no nuclei and finely granular and basophilic material in the cytoplasm because of calcification are known as ghost adipocytes [4]. In older lesions, fat necrosis and calcified ghost adipocytes are less evident. This liquefactive necrosis of adipocytes will clinically manifest as spontaneous discharge of oily brown material, which was evident in our patient when performing the biopsy.
The treatment of pancreatic panniculitis is directed at the underlying pancreatic disease. Usually those cases associated with pancreatitis slowly undergo resolution once the inflammatory episode of the pancreas regresses. When there is involvement of subcutaneous fat other than the lower extremities, persistent disease, frequent relapses, or ulceration, the possibility of an occult underlying carcinoma of the pancreas should be considered [1].
References
1. Luis Requena, Evaristo Sanchez Yus. Panniculitis. Part ii. Mostly lobular Panniculitis. J Am Acad Dermatol. 2001 Sep; 45(3):325-361. [PubMed]2. Dahl P R, Su W P, Cullimore K C, Dicken C H. Pancreatic panniculitis. J Am Acad Dermatol. 1996 Aug;35(2 Pt 1):282-3 . [PubMed]
3. Förström P L, Winkelmann R K. Acute grneralized panniculitis with Amylase and Lipase in the skin. Arch Dermatol. 1975 Apr; 111(4):497-502. [PubMed]
4. Lewis C T 3rd, Tschen J A, Klima M. Subcutaneous fat necrosis associated with pancreatic islet cell carcinoma. Am J Dermatopathol. 1992 Apr; 13(1):52-6. [PubMed]
© 2009 Dermatology Online Journal

