Leukemia cutis (chronic lymphocytic leukemia-low grade B cell)
Published Web Location
https://doi.org/10.5070/D37d87t9pgMain Content
Leukemia cutis (chronic lymphocytic leukemia-low grade B cell)
Chrysalyne A. Schmults
Dermatology Online Journal 8(2): 14
From New York University Department of DermatologyHistory
This 86-year-old man has a ten year history of a skin problem involving the left upper arm, right shoulder, right upper back, and right axilla. Although many of the present skin lesions have been present since 1990, some new lesions have gradually appeared over the past 10 years. Some lesions have resolved over time. They are asymptomatic. The lesions were first evaluated in August, 1990, and a punch biopsy was performed. Additional biopsy specimens were obtained in December, 1996 and November, 2000. The lesions have remained untreated since they are not bothersome and are slow to change. Chronic lymphocytic leukemia (low-grade B-cell) was diagnosed in 1986. The leukemia has never required treatment although the patient has hypersplenism with thrombocytopenia.
Past medical history includes atrial fibrillation, hypertension, congestive heart failure, chronic renal insufficiency, hypokalemia, transurethral prostatectomy, peripheral vascular disease with chronic stasis and edema of the lower extremities, portal venous congestion, and iron-deficiency anemia. Dermatologic history includes Grover's disease, basal-cell carcinoma, squamous-cell carcinoma, keratoacanthomas, porokeratosis of Mibelli, and actinic keratoses.
Physical Examination
 |  |
| Figure 1 | Figure 2 |
|---|
Several, erythematous-to-violaceous, rubbery nodules were present over the right upper back, shoulder, and axilla, and on the left upper arm.
Laboratory Data
White-count is stable at 20 x 109/L, hematocrit 34.9%, creatinine 1.6 mg/dl, total bilirubin 2.0 mg/dl, and direct bilirubin 0.5 mg/dl.
Histopathology
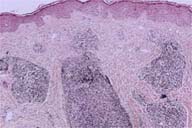
There is a superficial and deep, perivascular-to-nodular infiltrate of monotonous, small-to-medium-sized lymphocytes with hyperchromatic nuclei. Immunostains showed that these cells are B lymphocytes.
Comment
The incidence of leukemia cutis is not known since prospective studies have not been performed. In patients with acute myelogenous leukemia (AML) and myelodysplastic syndrome (MDS) biopsy specimens of the skin lesions show leukemia cutis in 25 percent of cases (the remainder show graft-versus-host disease, infection, drug reactions, or reactive infiltrates). Gingival and oral lesions with leukemic infiltrates are common in AML and are reported to occur in 50 percent of patients. In acute lymphatic leukemia (ALL), chronic myelogenous leukemia (CML), and chronic leukocytic leukemia, 50 percent of skin biopsies show leukemia cutis. Leukemia cutis was present in 25 to 30 percent of reported cases of congenital leukemia.
Erythematous-to-violaceous rubbery papules or nodules compromise 60 percent of cases of leukemia cutis overall, and infiltrated plaques compromise approximately one-fourth of cases. The remaining cases include uncommon manifestations, such as ecchymoses, palpable purpura, ulcers, urticaria , guttate psoriasiform lesions, annular forms (seen especially in juvenile CML), or erythema nodosum-like lesions. Lesions have been reported to occur at sites of previous herpes zoster or herpes simplex infections.
The lesions usually appear at the time of diagnosis or thereafter. It is uncommon for lesions to appear when peripheral blood and bone marrow are normal. However, one study reported that in MDS, 50 percent of leukemia cutis cases preceded blood or bone marrow evidence of leukemia . The authors proposed that leukemia cutis may be a marker for MDS patients who are likely to undergo leukemic transformation.
Overall, leukemia cutis is thought to be a poor prognostic marker with 90 percent of patients having extramedullary leukemic involvement and 40 percent having meningeal lesions. However, the data varies depending upon the type of leukemia. In congenital leukemia, prognosis is unaffected by the presence of leukemia cells. In B-cell chronic leukocytic leukemia, patients with predominantly (>95 percent) small B-lymphocyte infiltrates without reactive cells or epidermal changes had a two-year survival rate of 97 percent compared to 49 percent for all other biopsy specimens that did not meet these criteria. Five year survival was 67 percent overall. This survival rate was the same as that for B-cell chronic leukocytic leukemia without leukemia cutis. Treatment with intralesional interferon alpha and systemic chemotherapy can cause regression of lesions. Recurrence, however, is common.
References
Desch JK, et al. The spectrum of cutaneous disease in leukemias. J Cutan Pathol 20:407, 1993Longacre TA, et al. Leukemia cutis: analysis of 50 biopsy proven cases with an emphasis on occurrence in myelodysplastic syndromes. Am J Clin Pathol 100:276, 1993
Ratnam KV, et al. Leukemia cutis. Dermatol Clin 12:419, 1994
Su WP. Clinical, histopathological, and immunohistochemical correlations in leukemia cutis. Semin Dermatol 13:223, 1994
Cerroni L, et al. Specific cutaneous infiltrates of B-cell chronic lymphocytic leukemia: a clinicopathological and prognostic study of 42 patients. Am J Surg Pathol 20:1000, 1996
Kaddu S, et al. Prognostic evaluation of specific cutaneous infiltrates in B-chronic lymphocytic leukemia. J Cutan Pathol 23:487, 1996
© 2002 Dermatology Online Journal

