Lamotrigine induced subacute cutaneous lupus erythematous
Published Web Location
https://doi.org/10.5070/D371g1b76bMain Content
Letter: Lamotrigine induced subacute cutaneous lupus erythematous
M Cabanillas1 MD, O Suárez-Amor1 MD, A Ramírez-Santos1 MD, D González-Vilas1 MD, B Núñez-Acevedo2 MD, B Monteagudo1 PhD, C de las Heras1 MD
Dermatology Online Journal 18 (8): 12
1. Department of Dermatology, Complexo Hospitalario Arquitecto Marcide-Novoa Santos, Ferrol, Spain2. Department of Allergology, Complexo Hospitalario Universitario, Santiago de Compostela, Spain
Abstract
A 48-year-old woman developed drug-induced subacute lupus erythematosus while taking lamotrigine. The eruption resolved after discontinuance of lamotrigine, suggesting this drug as the cause.
Drug induced subacute cutaneous lupus erythematous (DI-SCLE) is a variant of lupus with predominant skin involvement, temporally related to drug exposure and resolving after drug discontinuation. DI-SCLE has been described in association with many different medications, most frequently hydroclorotiazide, antihypertensive agents, and terbinafine. We report a case of subacute cutaneous lupus erythematous that regressed after stopping lamotrigine, being used for epilepsy. This suggests a pathogenic role of this drug in the development of the disease.
 |  |
| Figure 1 | Figure 2 |
|---|
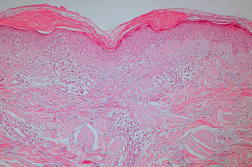
A 48-year-old woman presented in February 2010 with a 3-month history of a slightly itchy skin eruption involving the upper trunk and boths arms, which scarcely improved after treatment with oral corticosteroids and antihistamines. Fever, arthralgias, and malaise were not present. She had refractory primary generalized epilepsy, diagnosed 9 years before, for which she underwent medical treatment with lamotrigine (since 2006) combined with different drugs (levetiracetam in the previous 6 months). Four weeks before the onset of the eruption lamotrigine was increased from 400 mg/day to 500 mg/day. Examination revealed erythematous and scaly, annular plaques involving the trunk and proximal areas of the arms (Figure 1). Laboratory investigations revealed low titers of ANA (1/80), negative anti-Ro/SSA and anti-La/SSB antibodies, but positive anti-histone antibodies. Histological examination of a biopsy specimen of the lesions showed an interface dermatitis with focal vacuolization of the epidermal basal layer and apoptotic keratinocytes in the epidermis. There was a perivascular and periadnexal lymphohistiocytic infiltrate in the dermis. Lamotrigine was slowly decreased and finally stopped and replaced by valproic acid, continuing levetiracetam. Within 2 months, and with no other medical treatment, we observed a complete disappearance of the skin rash.
DI-SCLE has classically been described as a different entity from drug-induced systemic lupus erythematosus (DISLE). Clinically, DI-SCLE usually presents with annular or papulosquamous plaques, usually in a pattern that suggests photoexacerbation. In contrast, patients with DISLE rarely have dermatologic findings, but if present, they include malar erythema or photodistributed erythema. Patients with DI-SCLE rarely exhibit systemic symptoms, whereas patients with DISLE commonly have fever, malaise, arthralgia, polyarthritis, pericarditis, and pleuritis. Patients with DI-SCLE have anti-Ro/SSA antibodies and sometimes have anti-histone antibodies, whereas patients with DISLE have anti-histone antibodies and only rarely, if ever, anti-Ro/SSAþ. In addition, the drugs that are associated with these two entities differ. DI-SCLE is most often associated with HCTZ, antihypertensive agents, and terbinafine, whereas DISLE is most often associated with procainamide, hydralazine, isoniazid, and minocycline. Tumor necrosis factor-alpha antagonists have been associated with the development of both DI-SCLE and DISLE [1]. Lamotrigine is an anticonvulsivant agent that has been reported to induce systemic lupus in two different case reports [4, 5], but DI-SCLE has not been related with this drug to date in the literature.
Our case differs from the classical description of DI-SCLE in serological expression, which is more similar to DISLE: positive anti-Ro antibodies are usually present in DI-SCLE, but 20 percent of cases show negative titers, like ours. On the other hand, positive anti-histone antibodies are usually linked to DISLE, but they can be also positive in 33 percent of DI-SCLE [2]. In our opinion, these findings highlight that DISLE and DI-SCLE are not so different entities and there is probably a sort of overlap in some cases. However, the clinical and histological picture of our patient fits better with DI-SCLE; the widespread presentation of cutaneous lesions, similar to classical SCLE [3].
The incubation period was quite long in our case (4 years), although ranges in the literature from 3 weeks to 6 years have been reported [2]. The increase of the dose of lamotrigine seems to have been the trigger of the disease in our patient, although the idea of a dose-related effect of the drug in the development of this dermatosis is quite controversial. The pathogenetic mechanism of this condition is still unknown, although we agree with Callen that DI-SCLE probably represents an exacerbation of a pre-existing predisposition [1].
References
1. Callen JP. Drug-induced subacute cutaneous lupus erythematosus. Lupus. 2010;19:1107-11. [PubMed]2. Lowe G, Henderson CL, Grau RH, Hansen CB, Sontheimer RD. A systematic review of drug-induced subacute cutaneous lupus erythematosus. Br J Dermatol. 2011;164:465-72. [PubMed]
3. Marzano AV, Lazzari R, Polloni I, Crosti C, Fabbri P, Cugno M. Drug-induced subacute cutaneous lupus erythematosus: evidence for differences from its idiopathic counterpart. Br J Dermatol. 2011;165:335-41. [PubMed]
4. Ravindran V. Lamotrigine-induced lupus: a case report. Int J Rheum Dis. 2011;14:47-8. [PubMed]
5. Sarzi-Puttini P, Panni B, Cazzola M, Muzzupappa S, Turiel M. Lamotrigine-induced lupus. Lupus. 2000;9:555-7. [PubMed]
© 2012 Dermatology Online Journal

