Cerebriform nevus sebaceus: A rare entity
Published Web Location
https://doi.org/10.5070/D370m882b4Main Content
Cerebriform nevus sebaceus: A rare entity
Veena Maheshwari MD1, Kiran Alam MD1, Smriti Prasad MD1, Rajeev Sharma MD2, AH Khan MCh3, Preeti Sood MD1
Dermatology Online Journal 12 (7): 21
1. Department of Pathology, Jawaharlal Nehru Medical College and Bishen Skin Centre, Aligarh. saanjulimaheshwari@yahoo.co.uk2.
Department of Skin and Venereal Disease, Jawaharlal Nehru Medical College and Bishen Skin Centre 3. Department of Plastic
Surgery, Jawaharlal Nehru Medical College and Bishen Skin Centre
Abstract
We present a case of cerebriform nevus sebaceus in an 18-year-old boy. This form of nevus sebaceus is quite rare, in contrast to the relatively common linear variant.
Nevus sebaceus is a benign congenital hamartoma that is usually located on scalp or face as a single lesion. It appears as a plaque in childhood and becomes verrucous or nodular at puberty [1]. A cerebriform pattern of nevus sebaceus has been reported only once in recent literature [2].
Clinical synopsis

|

|
| Figure 1 | Figure 2 |
|---|---|
|
Figure 1. Cerebriform brownish nodular lesion on right parietal region Figure 2. Short black terminal hair seen in the sulci over the scalp |
|
An 18-year-old boy presented with a cerebriform, brownish, soft, mobile nodular plaque of 10 x 7 cm on the right parietal scalp, extending up to the superior occipital ridge (Fig. 1). It had multiple folds with short black terminal hair in the sulci (Fig. 2). Follicular plugging was present. Skeletal survey, neurological examination, and ophthalmological assessment were normal. The patient had a few small dark macules on the back (Fig. 3).

|
| Figure 3 |
|---|
| Multiple dark brown macules on the back |
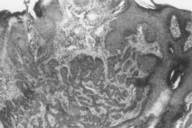
Skin biopsy revealed hypertrophy, acanthosis, and papillomatosis of the epidermis, findings consistent with the diagnosis of nevus sebaceus (Fig. 4). Marked proliferation of sebaceous glands was present in upper dermis (Fig. 5). Malformed hair follicles with follicular plugging were also present.
Discussion
Nevus sebaceus usually occurs as a solitary hamartoma located either on the scalp or on the face [3]. When extensive, these lesions may show evidence of a neurocutaneous syndrome (epilepsy and mental retardation, neurologic defects or skeletal abnormalities). None of these features were present in our patient [4]. The clinical importance of nevus sebaceus lesions stems from their propensity to develop secondary tumors, particularly basal cell carcinomas. In general, tumor formation does not occur until after puberty [5].
Secondary tumors may occur in these lesions. According to Chen et al., when that happens it is usually after age 10, with a mean age of 30 years [5]. The tumors identified were syringocystadenoma papilliferum, trichoblastoma, basal cell epithelioma, trichilemmoma, and sebaceus epithelioma. Multiple tumors developed in three cases of nevus sebaceus. Of the variety of tumors that may develop, most are benign. Many of the tumors previously classified as basal cell carcinoma are likely to have been trichoblastoma [6]. Hence, prophylactic removal, when feasible, or close followup with selected removal are options.
The development of squamous cell carcinoma within a nevus sebaceus is extremely rare, whereas the frequent association of nevus sebaceous with other appendage tumors and with apocrine glands suggests that nevus sebaceus is derived from the primary epithelial germ cells.
Most case reports of nevus sebaceus are of the linear form. Cerebriform nevus sebaceus is very rare and has been reported only once in the last 50 years [2]. The effective treatment in both types of nevus sebaceus is surgery and observation.
References
1. Lischner S. Dunsche A, Hauschild A. Congenital cerebriform nevus cell nevus on the occiput. Removal after tissue expander implantation. Hautarzt. 2001 Oct; 52 (10 pt2): 952-5.2. Ramesh A. Murugusundaram S. Vittel K. Kumar S, Janaki VR, and Boopalraj JM. Cerebriform sebaceous nevus. Int J Dermatol 1998; 37 (3): 220. PubMed
3. Van Geest AJ. Berretty PJ. Klirnkhamer PJ, Neumann HA. J. Eur. Acad Dermatol Venereol. 2002 Sep; 16 (5): 529-31. Cerebriform intradermal naevus (a rare form of secondary cutis verticis gyrata).
4. Ramos-e-Silva M. Martins G. Dadalti P. Maceira J. Cutis vertices gyrata secondary to a cerebriform intradermal nevus. Cutis. 2004 Apr; 73 (4): 254-6.
5. Chen MJ, Chan HL, Kuan YZ. Nevus sebaceus, -- a clinico pathological study of 104 cases. Chang Keng I Hsueh (TAIWAN) 1990; 13: 199-207.
6. Jaqueti G, Requena L, Sanchez Yus E. Trichoblastoma is the most common neoplasm developed in nevus sebaceus of Jadassohn: a clinicopathologic study of a series of 155 cases. Am J Dermatopathol. 2000;22:108-18.
© 2006 Dermatology Online Journal