Pachydermodactyly, a new case from Iran
Published Web Location
https://doi.org/10.5070/D36wd3p1jqMain Content
Pachydermodactyly, a new case from Iran
Abbas Zamanian MD1, Akram Ansar MD2
Dermatology Online Journal 17 (12): 8
1. Tehran University of Medical Sciences, Tehran, Iran2. Hamedan University of Medical Sciences, Hamedan, Iran
Abstract
Pachydermodactyly (PDD) is a rare form of benign digital fibromatosis involving the proximal portion of lateral sides of fingers. It is characterized by asymptomatic and symmetrical soft tissue swellings of the radial and ulnar aspects of proximal PIP joints of second to fifth fingers. Herein we report a 15-year-old boy with this condition.
Introduction
Pachydermodactyly is a benign form of digital fibromatosis with unknown etiology [1-5]. It is a rare disorder and only less than hundred cases have been reported in the literature [4]. Clinically it appears as a painless swelling of the soft tissues on the lateral aspects of the proximal interphalangial joints of the second to fifth fingers. It has been suggested that repeated rubbing of the fingers or mechanical injury to the joints may be contribute to the condition. Types 3 and 5 collagen are increased and electron microscopy shows increased numbers of fine-diameter collagen fibers. It is more common in adolescent males. We present here a new case from Iran.
Case report
 |  |
| Figure 1 | Figure 2 |
|---|
 |
| Figure 3 |
|---|
A 15-year-old boy presented to the dermatology clinic of Farshchian Hospital in Hamadan, in the west of Iran, with a painless enlargement of the lateral aspects of proximal interphalangial (PIP) joints of the second to fourth fingers on the right and left hands (Figures 1 and 2). He worked as a farmer with his father and described a one-year history of swelling of his PIP joints of both hands. The patient did not have pain, pruritus, restriction of movement, or morning stiffness. He had no other symptomatic complaints and upon systemic and dermatological examination, there were no other findings. Radiography of his hands showed swelling of the soft tissues around the fingers without bony abnormality. Routine laboratory tests were normal.
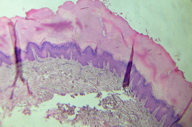
Histological examination of a biopsy specimen revealed epidermal hyperplasia, thickness of dermal collagen bundles, and an increased number of fibroblasts (Figure 3).
Discussion
Pachydermodactyly (PDD) is a rare form of benign digital fibromatosis involving the proximal portion of the lateral sides of the fingers. It is characterized by asymptomatic and symmetrical soft tissue swellings of the radial and ulnar aspects of the proximal PIP joints of the second to fifth fingers [1-7]. Young males are predominantly affected [1, 4, 9], but it has been reported in women and the elderly [3, 10-16]. Additional affected family members have been reported [15].
The exact etiology of pachydermodactyly remains unknown [5, 8]. However, some postulate that repetitive trauma or mechanical injury to the joints is a possible cause of the disorder, whereas others have suggested the psychological habit of interlacing the fingers [7]. We present a 15-year-old boy who we diagnosed as having PDD by the clinical manifestations and this was supported by a radiological study, histological examination of a skin biopsy, and negative routine laboratory tests. This patient also worked as a farmer.
Several types of this condition have been described, depending on topology, etiology, and pathological associations [7]. PDD may be misdiagnosed as arthritis or knuckle pads. Pachydermodactyly should be distinguished from occupational callosities, obsessive “chewing pads,” and true knuckle pads. The differential diagnoses include knuckle pads, foreign body granuloma, chewing pads, collagenous plaques of the hands, juvenile digital fibromatosis, progressive nodular fibrosis of the skin, thyroid disease, pachydermoperiostosis (Touraine-Solente-Golé syndrome), acromegaly, connective tissue nevi, fibrosing inflammatory conditions, Garrod pads in violinists, acropachydermodactyly in psoriasis, paraneoplastic acropachydermodactyly, Thiemann disease, and sarcomas. In addition, all arthropathies involving the PIP joints should be considered, especially juvenile chronic arthritis and juvenile rheumatoid arthritis [17, 18, 19]. There is one report that described knuckle pads and PDD coexisting in one family [8]. Histological examination of a biopsy specimen from affected fingers showed mostly epidermal hyperplasia, bundles of thickened collagen within a sparsely cellular papillary and reticular dermis, and increased deposits of connective-tissue mucin [5, 8, 10, 17, 20], compatible with present study (Figure 3). Association with other disorders, including plantar pachydermy is reported [7], but we didn't find any such association in this patient. The cytology of the fibroblasts appeared benign. Isolation of collagen from the involved sites revealed collagen Types I, III, and V in a pattern typical of fibromatoses, with increased Types III and V. Compared with the collagen profile of the normal reticular dermis, increased numbers of fine-diameter collagen fibers were notable in electron micrographs [21].
Because of the benign course of PDD, most patients do not require therapy. However, some patients want to undergo treatment to rectify their appearance. Topical treatment with corticosteroids is ineffective. Intralesional injections of corticosteroids often provide good results. Psychological counseling is required for the individuals with compulsive behavior. In selected cases, surgical excision may be an effective cosmetic option [19]. We advised our patient to stop any mechanical skin irritation. As discussed above, a prompt diagnosis would prevent unnecessary investigations and avoid inappropriate treatment. It is necessary to remind dermatologists and rheumatologists about this disorder.
References
1. Al Hammadi A, Hakim M. Pachydermodactyly: case report and review of the literature. J Cutan Med Surg. 2007; 11(5):185-7. [PubMed]2. Sandobal C, Kuznietz A, Varizat A, Roverano S, Paira S. Pachydermodactyly: four additional cases. Clin Rheumatol. 2007; 26:962-4. [PubMed]
3. Bardazzi F, Neri I, Raone B, Patrizi A. Pachydermodactyly: seven new cases. Ann Dermatol Venereol. 1998; 125:247-50. [PubMed]
4. Ye S, Chen SL, Dong YQ, Lin F, Guo Q, Bao CD. Pachydermodactyly: six new cases from China. J Clin Rheumatol. 2005; 11:72-5. [PubMed]
5. Glicenstein J, Costa R. pachydermodactyly: a report of two cases. Chir Main. 2004; 23:205-7. [PubMed]
6. Anandacoomarasamy A, Bak HS, Peduto A, Manolios N. magnetic resonance imaging in Pachydermodactyly. J Rheumatol. 2005; 32: 2239-41. [PubMed]
7. Marcilly MC, Balme B, Luaute JP, Skoworn F, Berard F, Perrot H. Pachydermodactyly associated with plantar pachydermy. Ann Dermatol Venereol. 2003; 130: 777-80. [PubMed]
8. Chamberlin AJ, Venning VA, Wojnarowska F. Pachydermodactyly: a frome frusta of knukle pads? Australas J Dermatol. 2003; 44:140-3. [PubMed]
9. Cartier H, Guillet MH, Schollhammer M, Guillet G. Pachydermodactyly in adolescents: a sign of discomfort? Arch Pediatr. 1996; 3:1091-4. [PubMed]
10. Tompkins SD, McNutt NS, Shea CR. Distal pachydermodactyly. J Am Acad Dermatol. 1998; 38:359-62. [PubMed]
11. Draluck JC, Kopf AU, Hodak E. Pachydermodactyly: first report in a woman. J Am Acad Dermatol 1992; 27: 303-5. [PubMed]
12. Bardazzi F, Fanti PA, De Padova MP et al. Localized pachydermodactyly in a woman. Acta Derm Venereol Suppl (Stockh) 1994; 74: 152-3. [PubMed]
13. Kim TH, Cho YH, Park HB. Two cases of pachydermodactyly. J Dermatol. 1996 Jun; 23:419-24. [PubMed]
14. Cabanillas M, Monteagudo B, León-Muíños E, Suárez-Amor O. Pachydermodactyly in a Young Girl: Cutaneous Manifestation of a Psychiatric Disorder? Pediatric Dermatology 2010; 27:306-308 [PubMed]
15. Russo F, Rodriguez-Picardo A, Camacho F. Familial pachydermodactyly. Acta Derm Venereol 1994; 74: 386-7. [PubMed]
16. Bardazzi F, Neri I, Fanti PA, Patrizi A. Pachydermodactyly in Two Young Girls. Pediatric Dermatology 1996;13:288-291 [PubMed]
17. Kopera D, Soyer HP, Kerl H. An update on pachydermodactyly and a report of three additional cases. Br J Dermatol 1995; 133: 433-7. [PubMed]
18. Lautenschlager S, Itin PH, Rufli T. Pachydermodactyly: reflecting obsessive-compulsive behavior? Arch Dermatol 1994; 130: 387. [PubMed]
19. Seo SH, Sung HW. A Case of Pachydermodactyly. Ann Dermatol. 2011; 23: 258-261. [PubMed]
20. Hunt R, Mandal R, Walters R, Schaffer JV. Pachydermodactyly. Dermatology Online Journal 2010; 16 (11):5 [PubMed]
21. Reichert CM, Costa J, Barsky SH, Claysmith AP, Liotta LA, Enzinger FM, Triche TJ. Pachydermodactyly. Clin Orthop Relat Res. 1985;194:252-7. [PubMed]
© 2011 Dermatology Online Journal

