Epidermodysplasia verruciform-like Lesions in an HIV patient
Published Web Location
https://doi.org/10.5070/D36ks5t6qwMain Content
Epidermodysplasia verruciform-like Lesions in an HIV patient
David R Berk MD1, Anna L Bruckner MD1, Dongsi Lu MD PhD2
Dermatology Online Journal 15 (1): 1
1. Department of Dermatology, Stanford University School of Medicine, Stanford, California. dberk@stanford.edu2. Department of Pathology and Immunology, Washington University School of Medicine, St. Louis, Missouri
Abstract
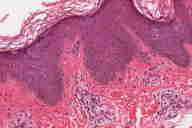
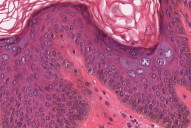
Epidermodysplasia verruciformis (EV) is a rare disorder involving widespread infection with specific human papillomavirus types and characteristic clinical lesions that may resemble verruca plana, tinea versicolor, psoriasis, or seborrheic keratoses. The most common HPV types found in EV are 5, 8, 17, and 20. Histopathologically, lesions demonstrate stereotypical enlarged keratinocytes in the upper epidermis with gray-blue cytoplasm, enlarged round nuclei with pale chromatin, and one or multiple nucleoli. Epidermodysplasia verruciformis may occur in either a classical form (often familial, early onset, and complicated by squamous cell carcinoma) or in association with various hereditary or acquired immunodeficiencies, particularly HIV. Fewer than 20 cases of HIV-associated epidermodysplasia verruciformis have been reported. We describe a 42-year-old HIV-positive man who presented with hypo- and hyperpigmented papules and plaques on the upper trunk, head, and neck, with histopathologic findings of epidermodysplasia verruciformis.
Case report
 |  |
| Figure 1a | Figure 1b |
|---|---|
| Figure 1. Hyper- and hypopigmented, thin, slightly verrucous papules and plaques on the face (1a), back (1b), and chest (1c). | |
 |
| Figure 1c |
|---|
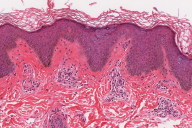
A 42 year-old HIV-positive African-American man presented with a 1-year history of asymptomatic hyper- and hypopigmented lesions, refractory to ketoconazole cream. He was on atazanavir, ritonavir, emtricitabine, and tenofovir and his CD4 count was 7 cells/mm³. Physical examination demonstrated thin, scaly, slightly verrucous hypo- and hyperpigmented papules and plaques on his head, neck, and upper trunk (Fig. 1). His hands were largely spared. Shave biopsy of a hyperpigmented plaque on his back revealed epidermal acanthosis with multifocal areas of altered keratinocytes arranged in small wedges in the granular and upper spinous layers. The altered keratinocytes have purple-blue cytoplasm, variable sized keratohyaline granules, enlarged round nuclei with pale chromatin, and one or multiple small nucleoli (Figure 2). A diagnosis of HIV-associated epidermodysplasia verruciform (EV) was made.
 |
| Figure 2c |
|---|
Discussion
Epidermodysplasia verruciformis may occur in either a classical, often hereditary form or in association with various hereditary or acquired immunodeficiencies. Patients with EV demonstrate infection with specific human papillomavirus (HPV) types and develop characteristic verrucous, premalignant clinical lesions. In classical EV, patients usually present in childhood with verruca plana-like lesions (often red-brown) on the extremities (especially dorsal hands), face, and neck [1, 2, 3]. A subset of patients may present as young adults [3]. Patients also often develop tinea versicolor-like lesions on the trunk, psoriasis-like lesions on the elbows, and/or seborrheic keratosis-like lesions on the forehead, neck, and trunk [4]. Lesions of EV have a stereotypical histopathologic appearance characterized by distinctive keratinocytes in the upper epidermis with gray-blue cytoplasm, enlarged round nuclei with pale chromatin and one or multiple small nucleoli. Epidermodysplasia verruciformis-associated HPV types include 3 and 10 (both typical of verruca plana in non-EV patients) as well as types more unique to EV such as 5, 8, 9, 12, 14, 15, 17, 19-25, 36-38, 47, and 50 (beta-HPVs). Individual EV patients often demonstrate multiple HPV types in their lesions and the most commonly identified HPV types depend on the molecular techniques used. Overall, HPV types 5, 8, 17, and 20 have most commonly been identified but the significance of more recently discovered HPV types remains poorly characterized [5]. Human papillomavirus types 5 and 8 are closely associated with malignant EV lesions. Classical hereditary EV may be caused by autosomal recessive defects in EVER1/TCM6 or EVER2/TCM8, both of which are located on chromosome 17 (near a psoriasis susceptibility locus) and encode integral membrane proteins of unknown function in the endoplasmic reticulum [6]. A second susceptibility locus has been mapped to chromosome 2 (near another psoriasis susceptibility locus), although the specific gene defect is still undiscovered [7]. Finally, several pedigrees with classical EV have suggested the existence of an X-linked recessive form of transmission [8, 9].
Squamous cell carcinoma (SCC) develops in 30-60 percent of EV patients on sun-exposed surfaces usually beginning between 20-40 years of age. Darkly pigmented EV patients are highly protected from SCC [10]. The vast majority of EV-associated SCCs are associated with HPV types 5 and 8, although HPV types 14 and 47 may also be important. Epidermodysplasia verruciformis patients who have lower production of interleukin-10 genotypes are predisposed to develop SCC [11]. Epidermodysplasia verruciformis-associated SCCs may be quite locally destructive but infrequently metastasize. Actinic keratoses, Bowen disease, and basal cell carcinomas are other possible complications. Rarely, extracutaneous malignancies have been associated with EV [12, 13, 14]. Epidermodysplasia verruciformis patients have impaired cell-mediated immunity and cannot be sensitized to topical immunosensitizers [15, 16, 17].
Management of EV includes strict photoprotection and regular clinical surveillance for SCC. When possible, SCC should be surgically excised. Radiation therapy is contraindicated [3,18]. If skin grafts are required, they should be taken from photoprotected areas. Other approaches include topical and oral retinoids, topical calcipotriol, photodynamic therapy, cidofovir, cimetidine, interferon alpha-2a, 5-fluorouracil, cryotherapy, and imiquimod. However, in general, responses to these treatments have been either unsuccessful, inconsistent, or associated with rapid recurrence after treatment. The most commonly reported non-surgical treatments include systemic retinoids [2, 3, 19, 20, 21] or interferon [2, 3]. More recently, multiple patients have been treated with imiquimod with variable responses [3, 9, 22, 23, 24]. Although not studied systematically, the most effective non-surgical treatments which have reported may be combinational approaches with systemic or topical agents, such as acitretin and interferon [2, 3, 25, 26] and, more recently, interferon and imiquimod [23].
Although the importance of HPV in cervical SCC is well-documented, the role of HPV in cutaneous SCC is controversial [2]. Epidermodysplasia verruciformis may offer a model for cutaneous SCC [27] because (1) EV patients develop frequent SCC at early ages, (2) seroreactivity to EV-associated HPV is increased in non-EV patients with SCC [28, 29], and (3) transcriptionally active EV-associated HPV can often be detected in SCC in non-EV patients [30, 31], especially in immunosuppressed [32] and xeroderma pigmentosum patients [33], and particularly during the early stages of lesions (EV-associated HPV is more commonly found in actinic keratoses than SCCs) [34, 35]. However, EV-associated HPV has also been isolated from lesions of psoriasis [36], seborrheic keratoses [37], nevus sebaceous [38], epidermal inclusion cysts [39], HPV vulvitis [40], melanoma [41], and normal skin [42]. Interestingly, in immunocompetent individuals, sun exposure directly correlates with both EV-associated HPV positivity in clinically normal skin and EV-associated HPV seropositivity [43]. Nevertheless, it remains unclear whether EV-associated HPV directly causes SCC, serves as a co-factor (to ultraviolet radiation) in SCC development, only plays a role in early stages of SCC development, or is simply a bystander in actinic keratoses and SCC. In a recent case-control study, EVER2 polymorphisms were associated with SCC development [44]. Recent studies have also highlighted the potential transforming properties of several proteins coded by EV-associated HPV, such as HPV-8 E2 [45] and HPV-5 E6 [46]. The concept of the EV acanthoma (incidental EV-associated HPV in skin of non-EV patients) has been proposed [47], and may represent "field cancerization" (skin altered by EV-associated HPV, sunlight, and/or immunosuppression such that there is increased risk for tumor development) [48].
Epidermodysplasia verruciformis has been reported in various immunosuppressed states (sometimes referred to as "EV-like lesions") including HIV [9, 49-57], common variable immunodeficiency [58], graft versus host disease [59], renal transplantation [60], systemic lupus erythematosus [61], Hodgkin disease [62], WILD syndrome (warts, immunodeficiency, lymphedema, anogenital dysplasia) [63], and IgM deficiency [20, 64]. Of these conditions, HIV-associated EV has been most frequently described, although a recent case report and review [55] identified only 15 reported cases of HIV-associated EV and the largest series [49, 50, 51] of HIV-associated EV have included only 3 patients. The authors of that review noted that most patients with HIV-associated EV presented with typical hypopigmented tinea versicolor-like lesions on the upper trunk and face, and had previously received antifungal therapy. Unusual presentations of EV-like lesions or EV-associated HPV in HIV patients have included scaly, erythematous, flat papules and plaques in the groin [56] and associated cervical intraepithelial during immune restoration [65]. Because EV only rarely occurs in HIV patients, some authors have hypothesized that EV only arises in those HIV patients with as yet undefined genetic susceptibilities [52, 53, 54]. A report of EV in HIV-infected half-siblings supports this notion [9].
Our patient did not follow-up for treatment after his biopsy. Treatment is usually less successful in HIV-associated EV than in classical EV. In the largest series of HIV patients with EV, multiple modalities were attempted and found to be either ineffective or limited by recurrence after treatment [49, 50, 51]. Highly active antiretroviral therapy does not seem to significantly impact the course of disease [51, 53], although one case report highlighted improvement [57]. Finally, the rate of SCC in HIV-associated EV seems to be much less than in classical EV. We are not aware of a reported case of HIV-associated EV with malignant transformation [56].
References
1. de Oliveira WR, Festa Neto C, Rady PL, Tyring SK: Clinical aspects of epidermodysplasia verruciformis. J Eur Acad Dermatol Venereol 2003;17:394-398. [PubMed]2. Gewirtzman A, Bartlett B, Tyring S: Epidermodysplasia verruciformis and human papilloma virus. Curr Opin Infect Dis 2008;21:141-146. [PubMed]
3. Gul U, Kilic A, Gonul M, et al.: Clinical aspects of epidermodysplasia verruciformis and review of the literature. Int J Dermatol 2007;46:1069-1072. [PubMed]
4. Foong HB, Ibrahimi OA, Elpern DJ, et al.: Multiple facial seborrheic keratosis-like lesions in a young woman with epidermodysplasia verruciformis. Int J Dermatol 2008;47:476-478. [PubMed]
5. de Oliveira WR, He Q, Rady PL, et al.: HPV typing in Brazilian patients with epidermodysplasia verruciformis: high prevalence of EV-HPV 25. J Cutan Med Surg 2004;8:110-115. [PubMed ]
6. Ramoz N, Rueda LA, Bouadjar B, et al.: Mutations in two adjacent novel genes are associated with epidermodysplasia verruciformis. Nat Genet 2002;32:579-581. [PubMed]
7. Ramoz N, Taieb A, Rueda LA, et al.: Evidence for a nonallelic heterogeneity of epidermodysplasia verruciformis with two susceptibility loci mapped to chromosome regions 2p21-p24 and 17q25. J Invest Dermatol 2000;114:1148-1153. [PubMed]
8. Androphy EJ, Dvoretzky I, Lowy DR: X-linked inheritance of epidermodysplasia verruciformis. Genetic and virologic studies of a kindred. Arch Dermatol 1985;121:864-868. [PubMed]
9. Hu W, Nuovo G, Willen M, Somach S: Epidermodysplasia verruciformis in two half brothers with HIV infection. J Cutan Med Surg 2004;8:357-360. [PubMed]
10. Jacyk WK, Subbuswamy SG: Epidermodysplasia verruciformis in Nigerians. Dermatologica 1979;159:256-265. [PubMed]
11. de Oliveira WR, Rady PL, Grady J, et al.: Polymorphisms of the interleukin 10 gene promoter in patients from Brazil with epidermodysplasia verruciformis. J Am Acad Dermatol 2003;49:639-643. [PubMed]
12. Slawsky LD, Gilson RT, Hockley AJ, Libow LF: Epidermodysplasia verruciformis associated with severe immunodeficiency, lymphoma, and disseminated molluscum contagiosum. J Am Acad Dermatol 1992;27:448-450. [PubMed]
13. Youssef M, Denguezli M, Ghariani N, et al.: Epidermodysplasia verruciformis associated with intestinal lymphoma: a model of viral oncogenicity. Pediatr Dermatol 2007;24:511-513. [PubMed]
14. Majewski S, Jablonska S: Human papillomavirus-associated tumors of the skin and mucosa. J Am Acad Dermatol 1997;36:659-685; quiz 686-658. [PubMed]
15. Glinski W, Obalek S, Jablonska S, Orth G: T cell defect in patients with epidermodysplasia verruciformis due to human papillomavirus type 3 and 5. Dermatologica 1981;162:141-147. [PubMed]
16. Majewski S, Skopinska-Rozewska E, Jablonska S, et al.: Partial defects of cell-mediated immunity in patients with epidermodysplasia verruciformis. J Am Acad Dermatol 1986;15:966-973. [PubMed]
17. Majewski S, Malejczyk J, Jablonska S, et al.: Natural cell-mediated cytotoxicity against various target cells in patients with epidermodysplasia verruciformis. J Am Acad Dermatol 1990;22:423-427. [PubMed]
18. Cortes-Franco R, Tyring SK, Vega E, et al.: Divergent clinical course of epidermodysplasia verruciformis in siblings. Int J Dermatol 1997;36:442-445. [PubMed]
19. Kanerva LO, Johansson E, Niemi KM, et al.: Epidermodysplasia verruciformis. Clinical and light- and electron-microscopic observations during etretinate therapy. Arch Dermatol Res 1985;278:153-160. [PubMed ]
20. Iraji F, Faghihi G: Epidermodysplasia verruciformis: association with isolated IgM deficiency and response to treatment with acitretin. Clin Exp Dermatol 2000;25:41-43. [PubMed]
21. Rallis E, Papatheodorou G, Bimpakis E, et al.: Systemic low-dose isotretinoin maintains remission status in epidermodysplasia verruciformis. J Eur Acad Dermatol Venereol 2008;22:523-525. [PubMed]
22. Janssen K, Lucker GP, Houwing RH, van Rijssel R: Epidermodysplasia verruciformis: unsuccessful therapeutic approach with imiquimod. Int J Dermatol 2007;46 Suppl 3:45-47. [PubMed]
23. Baskan EB, Tunali S, Adim SB, et al.: A case of epidermodysplasia verruciformis associated with squamous cell carcinoma and Bowen's disease: a therapeutic challenge. J Dermatolog Treat 2006;17:179-183. [PubMed]
24. Berthelot C, Dickerson MC, Rady P, et al.: Treatment of a patient with epidermodysplasia verruciformis carrying a novel EVER2 mutation with imiquimod. J Am Acad Dermatol 2007;56:882-886. [PubMed]
25. Anadolu R, Oskay T, Erdem C, et al.: Treatment of epidermodysplasia verruciformis with a combination of acitretin and interferon alfa-2a. J Am Acad Dermatol 2001;45:296-299. [PubMed]
26. Gubinelli E, Posteraro P, Cocuroccia B, Girolomoni G: Epidermodysplasia verruciformis with multiple mucosal carcinomas treated with pegylated interferon alfa and acitretin. J Dermatolog Treat 2003;14:184-188. [PubMed]
27. Majewski S, Jablonska S: Epidermodysplasia verruciformis as a model of human papillomavirus-induced genetic cancer of the skin. Arch Dermatol 1995;131:1312-1318. [PubMed]
28. Feltkamp MC, Broer R, di Summa FM, et al.: Seroreactivity to epidermodysplasia verruciformis-related human papillomavirus types is associated with nonmelanoma skin cancer. Cancer Res 2003;63:2695-2700. [PubMed]
29. Masini C, Fuchs PG, Gabrielli F, et al.: Evidence for the association of human papillomavirus infection and cutaneous squamous cell carcinoma in immunocompetent individuals. Arch Dermatol 2003;139:890-894. [PubMed]
30. Purdie KJ, Surentheran T, Sterling JC, et al.: Human papillomavirus gene expression in cutaneous squamous cell carcinomas from immunosuppressed and immunocompetent individuals. J Invest Dermatol 2005;125:98-107. [PubMed]
31. Forslund O, Ly H, Reid C, Higgins G: A broad spectrum of human papillomavirus types is present in the skin of Australian patients with non-melanoma skin cancers and solar keratosis. Br J Dermatol 2003;149:64-73. [PubMed]
32. Harwood CA, Surentheran T, McGregor JM, et al.: Human papillomavirus infection and non-melanoma skin cancer in immunosuppressed and immunocompetent individuals. J Med Virol 2000;61:289-297. [PubMed]
33. Luron L, Avril MF, Sarasin A, Daya-Grosjean L: Prevalence of human papillomavirus in skin tumors from repair deficient xeroderma pigmentosum patients. Cancer Lett 2007;250:213-219. [PubMed]
34. Pfister H, Fuchs PG, Majewski S, et al.: High prevalence of epidermodysplasia verruciformis-associated human papillomavirus DNA in actinic keratoses of the immunocompetent population. Arch Dermatol Res 2003;295:273-279. [PubMed]
35. Weissenborn SJ, Nindl I, Purdie K, et al.: Human papillomavirus-DNA loads in actinic keratoses exceed those in non-melanoma skin cancers. J Invest Dermatol 2005;125:93-97. [PubMed]
36. Weissenborn SJ, Hopfl R, Weber F, et al.: High prevalence of a variety of epidermodysplasia verruciformis-associated human papillomaviruses in psoriatic skin of patients treated or not treated with PUVA. J Invest Dermatol 1999;113:122-126. [PubMed]
37. Li YH, Chen G, Dong XP, Chen HD: Detection of epidermodysplasia verruciformis-associated human papillomavirus DNA in nongenital seborrhoeic keratosis. Br J Dermatol 2004;151:1060-1065. [PubMed]
38. Carlson JA, Cribier B, Nuovo G, Rohwedder A: Epidermodysplasia verruciformis-associated and genital-mucosal high-risk human papillomavirus DNA are prevalent in nevus sebaceus of Jadassohn. J Am Acad Dermatol 2008;59:279-294. [PubMed]
39. Ramagosa R, de Villiers EM, Fitzpatrick JE, Dellavalle RP: Human papillomavirus infection and ultraviolet light exposure as epidermoid inclusion cyst risk factors in a patient with epidermodysplasia verruciformis? J Am Acad Dermatol 2008;58:S68 e61-66. [PubMed]
40. Lin MT, Rohwedder A, Mysliborski J, et al.: 'HPV vulvitis' revisited: frequent and persistent detection of novel epidermodysplasia verruciformis-associated HPV genotypes. J Cutan Pathol 2008;35:259-272. [PubMed]
41. Rohwedder A, Slominski A, Wolff M, et al.: Epidermodysplasia verruciformis and cutaneous human papillomavirus DNA, but not genital human papillomavirus DNAs, are frequently detected in vulvar and vaginal melanoma. Am J Dermatopathol 2007;29:13-17. [PubMed]
42. Antonsson A, Erfurt C, Hazard K, et al.: Prevalence and type spectrum of human papillomaviruses in healthy skin samples collected in three continents. J Gen Virol 2003;84:1881-1886. [PubMed]
43. Termorshuizen F, Feltkamp MC, Struijk L, et al.: Sunlight exposure and (sero)prevalence of epidermodysplasia verruciformis-associated human papillomavirus. J Invest Dermatol 2004;122:1456-1462. [PubMed]
44. Patel AS, Karagas MR, Pawlita M, et al.: Cutaneous human papillomavirus infection, the EVER2 gene and incidence of squamous cell carcinoma: a case-control study. Int J Cancer 2008;122:2377-2379. [PubMed]
45. Pfefferle R, Marcuzzi GP, Akgul B, et al.: The human papillomavirus type 8 E2 protein induces skin tumors in transgenic mice. J Invest Dermatol 2008;128:2310-2315. [PubMed]
46. Mendoza JA, Jacob Y, Cassonnet P, Favre M: Human papillomavirus type 5 E6 oncoprotein represses the transforming growth factor beta signaling pathway by binding to SMAD3. J Virol 2006;80:12420-12424. [PubMed]
47. Ko CJ, Iftner T, Barr RJ, Binder SW: Changes of epidermodysplasia verruciformis in benign skin lesions: the EV acanthoma. J Cutan Pathol 2007;34:44-48. [PubMed]
48. Rohwedder A, Foong H, Tyring SK, et al.: Incidental epidermodysplasia verruciformis human papillomavirus infection (EV acanthoma): evidence for 'field cancerization' and a putative cofactor in seborrheic keratosis. J Cutan Pathol 2008. [PubMed]
49. Berger TG, Sawchuk WS, Leonardi C, et al.: Epidermodysplasia verruciformis-associated papillomavirus infection complicating human immunodeficiency virus disease. Br J Dermatol 1991;124:79-83. [PubMed]
50. Barzegar C, Paul C, Saiag P, et al.: Epidermodysplasia verruciformis-like eruption complicating human immunodeficiency virus infection. Br J Dermatol 1998;139:122-127. [PubMed]
51. Rallis E, Paparizos V, Kyriakis K, Katsambas A: Treatment of epidermodysplasia verruciformis in human immunodeficiency virus-positive patients. J Eur Acad Dermatol Venereol 2008. [PubMed]
52. Davison SC, Francis N, McLean K, Bunker CB: Epidermodysplasia verruciformis-like eruption associated with HIV infection. Clin Exp Dermatol 2004;29:311-312. [PubMed]
53. Carre D, Dompmartin A, Verdon R, et al.: Epidermodysplasia verruciformis in a patient with HIV infection: no response to highly active antiretroviral therapy. Int J Dermatol 2003;42:296-300. [PubMed]
54. Bonamigo R, Maldonado G, Londero RM, Cartell A: Epidermodysplasia verruciformis-like disorder in a teenager with HIV and HCV infections. Pediatr Dermatol 2007;24:456-457. [PubMed]
55. Hultgren TL, Srinivasan SK, DiMaio DJ: Epidermodysplasia verruciformis occurring in a patient with human immunodeficiency virus: a case report. Cutis 2007;79:307-311. [PubMed]
56. Trauner MA, Ruben BS, Hatcher SL, Lawry MA: Groin eruption in an HIV-positive man: epidermodysplasia verruciformis (EDV). Arch Dermatol 2002;138:527-532. [PubMed]
57. Haas N, Fuchs PG, Hermes B, Henz BM: Remission of epidermodysplasia verruciformis-like skin eruption after highly active antiretroviral therapy in a human immunodeficiency virus-positive patient. Br J Dermatol 2001;145:669-670. [PubMed]
58. Vu J, Wallace GR, Singh R, et al.: Common variable immunodeficiency syndrome associated with epidermodysplasia verruciformis. Am J Clin Dermatol 2007;8:307-310. [PubMed]
59. Kunishige JH, Hymes SR, Madkan V, et al.: Epidermodysplasia verruciformis in the setting of graft-versus-host disease. J Am Acad Dermatol 2007;57:S78-80. [PubMed]
60. Blessing K, McLaren KM, Benton EC, et al.: Histopathology of skin lesions in renal allograft recipients--an assessment of viral features and dysplasia. Histopathology 1989;14:129-139. [PubMed]
61. Yutsudo M, Kanda R, Tanigaki T, et al.: Human papillomavirus type 38 isolated from patients with epidermodysplasia verruciformis. Intervirology 1986;26:104-108. [PubMed]
62. Gross G, Ellinger K, Roussaki A, et al.: Epidermodysplasia verruciformis in a patient with Hodgkin's disease: characterization of a new papillomavirus type and interferon treatment. J Invest Dermatol 1988;91:43-48. [PubMed]
63. Kreuter A, Hochdorfer B, Brockmeyer NH, et al.: A human papillomavirus-associated disease with disseminated warts, depressed cell-mediated immunity, primary lymphedema, and anogenital dysplasia: WILD syndrome. Arch Dermatol 2008;144:366-372. [PubMed]
64. Gul U, Soylu S, Yavuzer R: Epidermodysplasia verruciformis associated with isolated IgM deficiency. Indian J Dermatol Venereol Leprol 2007;73:420-422. [PubMed]
65. Mermet I, Guerrini JS, Cairey-Remonnay S, et al.: Cervical intraepithelial neoplasia associated with epidermodysplasia verruciformis HPV in an HIV-infected patient: a manifestation of immune restoration syndrome. Eur J Dermatol 2007;17:149-152. [PubMed]
© 2009 Dermatology Online Journal