Localized cutaneous T cell lymphoma presenting as disfiguring facial lesions
Published Web Location
https://doi.org/10.5070/D36f52t9w4Main Content
Localized cutaneous T cell lymphoma presenting as disfiguring facial lesions
Feroze Kaliyadan MD DNB MNAMS1, Jayasree MG MD2, Manoj Unni MD DM3, Neeraj S MD4
Dermatology Online Journal 15 (11): 14
1. Associate Professor, Department of Dermatology, Amrita Institute of Medical Sciences, Kochi, Kerala, India 682028. ferozkal@hotmail.com2. Assistant Professor, Department of Pathology, Amrita Institute of Medical Sciences, Kochi, Kerala, India 682028
3. Associate Professor, Department of Oncology, Amrita Institute of Medical Sciences, Kochi, Kerala, India 682028
4. Senior Resident, Department of Hematology, CMC, Vellore, India
Abstract
We report a case of a 27-year-old male patient with localized cutaneous T cell lymphoma presenting as disfiguring lesions on the face.
Case report
A 27-year-old male patient presented with an asymptomatic nodular swelling, associated with scaling, over the forehead. The tumor had been slowly increasing in size over the last eleven years. The patient had had consultations at multiple centers and the growth had been biopsied at least three times in the past. Based on previous reports the patient had been treated under various different diagnoses, including cutaneous pseudo-lymphoma. The patient had been given both systemic and intra-lesional steroids for the same with no significant improvement. There was no history of any significant co-morbidity and had he had been extensively evaluated previously for the presence of any systemic illness. All his previous laboratory reports were within normal limits. Previous radiological studies including CT scan (head and neck) showed only soft tissue swelling with no deeper involvement.
 |
| Figure 1 |
|---|
| Figure 1. Extensive nodular lesions on forehead |
On examination the forehead showed an extensive firm swelling with prominent nodules on the surface and alopecia. The tumor extended around the eyelids especially over the left side. (Fig. 1) Moderate scaling was present. Some enlarged, comedo-like follicular infundibula were also seen in some areas. There was no evident oozing or crusting. There were no other significant skin or mucosal lesions elsewhere. There was no significant lymphadenopathy.
Systemic examination did not reveal any significant abnormality.
 |  |
| Figure 2 | Figure 3 |
|---|---|
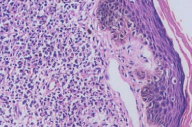
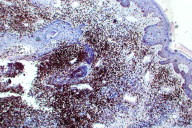
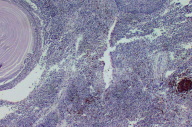
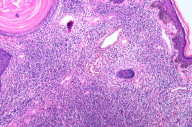
| Figure 2. Epidermotropism (H&E, x100) Figure 3. CD3 stain showing predominant CD3 positive cells (x4) | |
 |  |
| Figure 4 | Figure 5 |
|---|---|
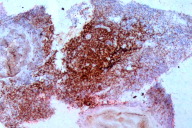
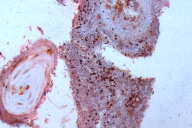
| Figure 4. CD4 stain showing most of the cells to be CD4 positive Figure 5. CD8 stain showing negativity for CD8 | |
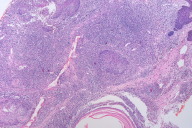
A deep skin biopsy was taken from the forehead. The biopsy showed hyperkeratosis with a few horn cysts. Epidermotropism was seen. The dermis showed a dense mono-morphic lymphocytic infiltrate. There was also no evidence of any significant dermal edema, spongiosis, extravasated erythrocytes, necrotic keratinocytes or epidermal eosinophilic infiltration. These negative findings are in concordance with the findings of Choi et al, who analyzed in detail the histological differences that distinguish a true lymphoma from a pseudolymphoma [1]. Immuno-histochemistry showed that the cells were predominantly CD 3; CD 4 positive and CD 8; CD20 negative. (Figs. 2 through 8) CD 30 and CD 56 were also negative. Gene rearrangement studies were not done.
 |  |
| Figure 6 | Figure 7 |
|---|---|
| Figure 6. CD20 showing negativity Figure 7. Dense monomorphic lymphocytc infiltrate (H&E, x100) | |
 |  |
| Figure 8 | Figure 9 |
|---|---|
| Figure 8. Dense lymphocytic infiltrate Figure 9. Post chemotherapy and radiation | |
Other laboratory investigations, including bone-marrow aspiration and biopsy, were within normal limits, except for a significantly raised Immunoglobulin E (1152 IU/ml N: 0.0 - 100.0) and a slightly elevated Lactate Dehydrogenase (280.2 U/L; normal 0.0 - 240.0). The initial peripheral blood smear was essentially normocytic, normochromic, but there appeared to be isolated large lymphocytes (otherwise typical). Radiological examination including chest-x-ray and ultrasound of the abdomen were within normal limits. Based on the histopathology and immunohistochemistry, a diagnosis of cutaneous -T -cell lymphoma (tumefactive stage of mycosis fungoides) was made. Even though the skin lesions were localized, the presence of a small number (< 5%) of large (but otherwise typical lymphocytes ) and the depth of the tumor shifted opinion in favor of initiating chemotherapy, rather than radiation therapy. The patient was started on chemotherapy (four cycles of CHOP regime - Adriamycin 80 mg, Vincristine 2 mg, cyclophosphamide 1280 mg and Prednisone 100 mg daily for five days). On follow up too, investigations did not show any evidence to suggest internal involvement. Follow up peripheral blood smears were normal. Considering the facts that the disease had not cleared completely and that the patient did not show any evidence of systemic involvement, the patient was put on local radiotherapy. (Teletherapy treatment technique: 3D conformal radiotherapy using conventional fractionation.) The patient received a total dose of 3000cGy in 15 fractions each to face and neck.There was further regression of the tumor size, but we still could not achieve complete clearance. (Fig. 9) The patient is under follow up and we are exploring the possibility of interferon therapy as an alternative.
Discussion
Unilesional Mycosis Fungoides (MF) is considered to be a rare variant of CTCL, affecting any age group, including children. The histopathological and immunophenotypical features are in general indistinguishable from those observed in multilesional MF. There may occasionally be cutaneous spread with the appearance of noncontiguous tumors, even a long time after therapy. Whether all cases represent minimal-stage IA MF or whether some are actually T cell pseudolymphoma remains to be clarified [2]. Classically tumors of unilesional MF are in the form of solitary eczematous plaques. Localized forms of small to medium sized pleomorphic cutaneous T cell lymphomas have also been described. The significance being that these lesions tend to remain stable for a very long time [3].
The other diagnosis to be considered in our case, especially considering the location of the lesions, would be folliculotropic MF. Mycosis fungoides lesions affecting the scalp and simulating follicular mucinosis have been described in the context of folliculotropic MF. Follicular MF differs from alopecia mucinosa with regard to its clinical presentation, histology and, presumably, prognosis. Characteristic findings of follicular MF include infiltrated plaques showing numerous enlarged, comedo-like follicular infundibula and a histology showing folliculotropism of atypical lymphocytes, sometimes forming follicular Pautrier microabscesses [4, 5]. Our case had no significant folliculotropism histologically. Hence we feel that our case represents a presentation of MF as an extensive localized nodule with disfigurement of the face. Iraji et al. have reported a similar case of cutaneous T cell lymphoma localized to the chest area [6]. This case is presented because of the extensive tumor with facial disfigurement and to highlight the point that even tumoral cutaneous T cell lymphoma can be localized for long periods of time. A high index of suspicion is therefore essential for diagnosis of this potentially lethal disease. The long history of localized disease was the most salient feature in our case.
Acknowledgement: We would like to thank the Dept of Pathology, CMC Vellore for their valuable help in obtaining CD4/CD8 immunohistochemistry.
References
1. Choi TS, Doh KS, Kim SH, Jang MS, Suh KS, Kim ST. Clinicopathological and genotypic aspects of anticonvulsant-induced pseudolymphoma syndrome. Br J Dermatol 2003; 148:730-6. [PubMed]2. Hodak E, Phenig E, Amichai B, Feinmesser M, Kuten A, Maron L, Sahar D, Bergman R, David M. Unilesional mycosis fungoides: a study of seven cases. Dermatology 2000; 201:300-6. [PubMed]
3. von den Driesch P, Coors EA. Localized cutaneous small to medium-sized pleomorphic T-cell lymphoma: a report of 3 cases stable for years. J Am Acad Dermatol 2002;46:531-5. [PubMed]
4. Klemke CD, Dippel E, Assaf C, Hummel M, Stein H, Goerdt S, Orfanos CE.
Follicular mycosis fungoides. Br J Dermatol 1999;141:137-40. [PubMed]
5. Roesch A, Schleyer V, Landthaler M, Vogt T. Follicular mycosis fungoides: variability of a rare entity. Skinmed 2005; 4:12-7. [PubMed]
6. Iraji F, Asilian A, Siadat AH, Rajabi P, Arbabi A. Unilateral mycosis fungoides. Dermatol Online J. 2008 ;14:25. [PubMed]
© 2009 Dermatology Online Journal

