A misdiagnosed nail bed melanoma
Published Web Location
https://doi.org/10.5070/D36dq4k8sbMain Content
A misdiagnosed nail bed melanoma
Amel Elloumi-Jellouli, Salma Triki, M Driss, F Derbel, Mohammed Zghal, K Mrad, Kh Ben Rhomdhnane
Dermatology Online Journal 16 (7): 13
Hôpital FSI, La Marsa, Tunis, Tunisia. amel.elloumi@yahoo.frAbstract
Nail bed melanoma or subungual melanoma is frequently misdiagnosed compared to other melanoma in other anatomic sites. We report the case of a 48-year-old woman presenting with a dystrophic and pigmented lesion of her fourth finger nail. This initial presentation had been mistaken for onychomycosis, but biopsy of nail bed and nail matrix confirmed nail bed melanoma. This case is presented to help increase the awareness of atypical presentations of acral melanoma.
Case synopsis
 |
| Figure 1 |
|---|
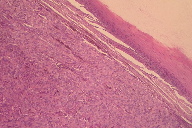
| Figure 1. Nail pigmented lesion |
A 48-year-old woman was referred to our department for a dystrophic and pigmented lesion of her fourth finger nail (Figure 1). She reported that the alteration of the nail pigmentation had begun 4 years prior. The nail was neither painful nor symptomatic. There was no personal or family history of melanoma. Her general practitioner diagnosed onychomycosis and treated it with a specific topical and oral treatment for 18 months with out any improvement. Physical examination of the fourth finger showed hyperkeratosis and pigmentation involving the entire nail plate. There was no visible pigmentation on either proximal nail fold or hyponychium. The rest of her fingernails appeared normal.
A radiograph of the digit demonstrated no abnormalities. A fungal culture of the nail plate revealed no growth. Biopsy specimens were taken from the nail bed and nail matrix.
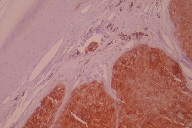
 |  |
| Figure 2c | Figure 2d |
|---|---|
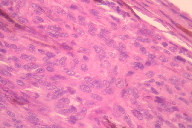
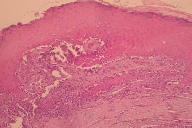
| Figure 2c. A lichenoid lymphocytic infiltrate was present at the periphery of the lesion. Figure 2d. Foci of necrosis are also present. | |
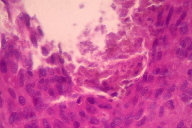
Pathological examination revealed atypical melanocytes in the nail bed and nail matrix; a diagnosis of subungual melanoma was made (Figures 2a through 2d). The melanoma extended to a Breslow depth of 3 mm. The atypical melanocytes were positive for HMB-45 (Figure 3) and for Melan A (Figure 4). The patient consequently underwent sentinel lymph node biopsy that proved to be negative.
 | 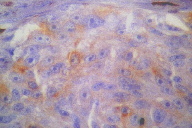 |
| Figure 3 | Figure 4 |
|---|---|
| Figure 3. Melan A positive Figure 4. HMB-45 positive | |
Amputation of the finger at the distal interphalangeal joint was performed. Final complete pathological examination confirmed that this tumor was a Clark Level IV melanoma. There has been neither recurrence nor metastasis 3 years after surgery.
Commentary
Subungual melanoma is a rare subtype of acral lentiginous melanoma with specific epidemiological characteristics. It represents 0.7 percent to 3.5 percent of cutaneous melanoma in Caucasians [1, 2]. It is generally associated with a poor prognosis and 85 percent of cases are misdiagnosed at the time of initial presentation [3]. The age distribution shows a peak incidence for the seventh decade of life, typically later than the other subtypes, except for lentigo malignant melanoma [4]. Often, it presents on the great toe or thumb as a longitudinal brown streak on the nail. This longitudinal melanonychia extends to the free margin and may cause nail dystrophy. Hutchinson sign is characterized by extension of pigmentation onto the nail fold and is considered to be the clinical phenotype of the radial growth phase [5]. However, this case shows that ungual melanoma may be advanced without showing Hutchinson sign.
For many years, melanoma of the nail area has been considered a deadly form of melanoma, with a reported 5-year overall survival of only 27 percent [6]. More recent studies, however, have reported 5-year overall survival ranging from 40 percent to 59 percent [7]. A review of 93 cases of subungual melanoma demonstrated that metastasis, histological thickness, patient’s race, and ulceration have prognostic value in predicting survival [8].
As is evident in this case, many factors seem to be responsible for the diagnosis delay. In the literature, subungual melanoma is not recognized in 15 percent to 20 percent of cases. This misdiagnosis often relates to lack of pigmentation in one-third of cases and an unusual presentation [4].
The primary misdiagnosis of a nail bed melanoma is onychomycosis. Clinical presentation of subungual melanoma starts typically with a longitudinal brown streak on the nail. This presentation is overlooked as a benign condition, such as subungual hematoma, bacterial infection, pyogenic granuloma, subungual verruca, subungual exostosis, glomus tumor, subungual nevus, or digital mucous cyst [9, 10]. Other tumors that can mimic amelanotic melanoma include acquired fibrokeratoma, Bowen disease, squamous cell carcinoma, eccrine syringofibroadenoma, and onychomatricoma.
Amputation of the distal phalanx must be considered the standard approach to treatment of the primary lesion for thick melanoma. Margins of excision used for patients with other types of melanoma should be practiced. Patients with early lesions could be treated with conservative surgical treatment. Clinical follow-up of these patients is required.
Conclusion
The diagnosis of nail bed melanoma is often delayed. It must be taken into consideration in the differential diagnosis of all nail lesions, but more so in the elderly. An incisional biopsy of the nail matrix in involved areas is recommended.
References
1. Levit EK, Kagen MH, Scher RK, Grossman M, Altman E. The ABC rule for clinical detection of subungual melanoma. J Am Acad Dermatol 2000;42:269-74. [PubMed]2. High WA, Quirey RA, Guillén DR, Munõz G, Taylor RS. Presentation, histopathologic findings, and clinical outcomes in 7 cases of melanoma in situ of the nail. Arch Dermatol 2004; 140(9) : 1102-6. [PubMed]
3. Arican O, Sasmaz S, Coban YK, Ciralik H. Subungual amelanotic malignant melanoma. Saudi Med J. 2006 Feb;27(2):247-9. [PubMed]
4. De Giorgi V, Sestini S, Massi D, Panelos J, Papi F, Dini M, Lotti T. Subungual melanoma: a particularly invasive "onychomycosis." J Am Geriatr Soc. 2007 Dec;55(12):2094-6. [PubMed]
5. Imakado S, SatoH, Hamada K. Two cases of subungual melanoma in situ. J Dermatol 2008; 35: 754-8 [PubMed]
6. Patterson RH, Helwig EB. Subungual malignant melanoma: a clinical-pathologic study. Cancer 1980; 46(9):2074-87. [PubMed]
7. Cohen T, Busam KJ, Patel A, Brady MS. Subungual melanoma: management considerations Am J Surg. 2008 Feb;195(2):244-8. [PubMed]
8. O’Leary JA, Berend KR, Johnson JL, Levin LS, Seigler HF. Subungual melanoma: a review of 93 cases with identification of prognostic variables. Clin Orthop Relat Res. 2000 Sep;(378):206-12. [PubMed]
9. Soon SL, Solomon AR Jr, Papadopoulos D, Murray DR, McAlpine B, Washington CV. Acral lentiginous melanoma mimicking benign disease: The Emory experience. J Am Acad Dermatol 2003; Feb 48(2): 183-8. [PubMed]
10. Harrington P, O’Kelly A, Trail IA, Freemont AJ. Amelanotic subungual melanoma mimicking pyogenic granuloma in the hand. J R Coll Surg Edinb 2002;47(4):638-40. [PubMed]
© 2010 Dermatology Online Journal