Pemphigus herpetiformis of age of onset at 6 years
Published Web Location
https://doi.org/10.5070/D36677332sMain Content
Letter: Pemphigus herpetiformis of age of onset at 6 years
Roy Moutran MD1, Ismael Maatouk MD1, Farid Stephan MD1, Eugenie Halaby MD1, Gerard Abadjian MD2, Roland Tomb MD PhD1
Dermatology Online Journal 17 (6): 10
1. Department of Dermatology, Hôtel Dieu de France, Beyrouth, Lebanon2. Department of Pathology, Hôtel Dieu de France, Beyrouth, Lebanon
Abstract
INTRODUCTION: Pemphigus herpetiformis is a rare entity that combines the clinical features of dermatitis herpetiformis with the immunologic and histological features of pemphigus. It generally affects adults and pediatric cases are uncommon. We report a case of pemphigus herpetiformis in a 6-year-old girl treated successfully with dapsone. OBSERVATION: A 6-year-old girl presented with a pruritic, erythematous and vesiculous eruption. Histological examination showed acantholysis of the medial and superficial parts of the epidermis. Direct immunofluorescence study revealed cell surface immunoglobulin G and C3 deposits and staining on the dermo-epidermal junction. The child was diagnosed as having pemphigus herpetiformis. DISCUSSION: Pemphigus herpetiformis produces clinically a pruritic and atypical eruption that resembles dermatitis herpetiformis, with standard histology and immunofluorescence patterns recalling those of pemphigus. Considered to have a good prognosis, it responds well to dapsone and/or to low dose oral corticosteroids. The age range of onset varies from 31 to 81 years according to studies, without a male or female predilection. This is a report of a 6-year-old girl presenting with pemphigus herpetiformis, successfully treated with dapsone for two years with no relapse.
Introduction
Pemphigus herpetiformis is a rare entity that combines the clinical features of dermatitis herpetiformis with the immunologic and histological features of pemphigus [1]. It usually affects adults. Rarely, the disease can affect children. The earliest age of onset reported in the literature is 5 years. That report described a female patient who did not have a clinical response to dapsone [2]. We report a case of pemphigus herpetiformis in a 6-year-old girl treated successfully with dapsone.
Case report
 |  |
| Figure 1 | Figure 2 |
|---|
A 6-year-old girl, born of unrelated parents, presented with a 3-month history of a pruritic eruption, which began on the trunk and then gradually extended to the face and extremities. Clinical examination showed vesicules and bullae on annular, polycyclic, and erythematous plaques, leaving residual hyperpigmentation (Figure 1). No oral mucosal involvement was present.
The remaining physical examination was otherwise normal. The diagnosis of dermatitis herpetiformis was suspected, leading the clinician to perform a skin biopsy and to refer for gastroenterology consultation to rule out celiac disease by duodenal biopsy. The latter came back negative.
The patient was treated with oral prednisone at a dose of 10 mg/day (0.3 mg/kg/day) with partial regression of the disease. Nevertheless, relapses were noted upon each dose reduction of steroids.
She was then referred to our department. We immediately performed a skin biopsy for histology and immunofluorescence studies.
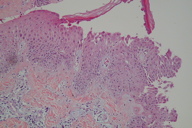
Histological examination showed an image of acantholysis affecting the middle and superficial layers of the epidermis with neutophilic infiltration (Figure 2). The dermis and hypodermis did not reveal abnormalities.
 |
| Figure 3 |
|---|
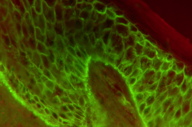
Direct immunofluorescence showed positive intercellular IgG and C3 staining throughout the epidermis and on the dermo-epidermal junction (Figure 3).
The diagnosis of pemphigus herpetiformis was established.
The patient was treated with dapsone at an initial dose of 2 mg/kg/day. Given the substantial improvement, the dose of prednisone was reduced gradually then stopped after 3 months of treatment. Dapsone has continued to be maintained (2 mg/kg/day) until now (24 months after the initial diagnosis). No relapses have been mentioned.
Discussion
The presentation of the skin eruption of the patient, its clinical appearance, and its histological picture (marked by acantholysis and characteristic deposition on direct immunofluorescence) suggest a particular form of pemphigus.
Pemphigus herpetiformis is an atypical form of auto-immune bullous diseases. It was first described in 1975 by Jablonska et al [3]. A study conducted on 205 cases of pemphigus described 15 cases of pemphigus herpetiformis (7.3%) [4].
Clinically, this disorder produces a pruritic and atypical eruption that resembles dermatitis herpetiformis. Standard histological examination (having low specificity and sensitivity) may show eosinophilic and/or neutrophilic spongiosis with or without suprabasal acantholysis [1, 5, 6].
Direct immunofluorescence (DIF) study reveals epidermic intercellular deposits of immunoglobulin G associated with occasional deposits of C3 [1]. Indirect immunofluorescence may show circulating IgG auto-antibodies directed against epithelial cells [1].
In our case, the DIF showed staining at the dermo-epidermal junction (DEJ), in addition to the classic intercellular pattern. This may be caused by the presence of the antigen on the basal part of the cytoplasmic membrane of the epidermal cells or by the presence of the same antigen in the DEJ.
The clinical picture reveals pruritic erythematous plaques, surrounded by a vesiculobullous ring, having a herpetiformis pattern that resembles dermatitis herpetiformis [1]. The responsible auto-antibodies are directed against desmoglein 1 and rarely against desmoglein 3 [7, 8], thus mucous membranes involvement is rare [9].
Pemphigus herpetiformis is considered to have a good prognosis and responds well to dapsone and/or to low dose oral corticosteroids. Some cases progress into pemphigus vulgaris or pemphigus foliaceus. The presence of circulating auto-antibodies is associated with a greater risk of resistance to treatment [1, 10].
Associations with neoplasms have been rarely reported; in a recent paper, anti-desmoglein 3 and an unknown 178-kDa protein were detected in a patient having pemphigus herpetiformis and lung carcinoma [11]. The average age of onset varies from 31 to 81 years according to studies, with no sex predilection [3, 12, 13]. Some pediatric cases have been published: 2 patients were 12 years old [14, 15], one girl was 10 [16], and a recent observation described a 5 year-old female having pemphigus herpetiformis who needed corticosteroids and immunosuppressive agents to induce remission [2].
This is a report of a 6-year-old girl presenting with pemphigus herpetiformis, successfully treated with dapsone for two years with no relapse.
References
1. Robinson N, Hashimoto T, Amagai M, Chan L. The new pemphigus variants. J Am Acad Dermatol 1999;40:649-71. [PubMed]2. Duarte IB, Bastazini I Jr, Barreto JA, Carvalho CV, Nunes AJ. Pemphigus herpetiformis in childhood. Pediatr Dermatol. 2010;27(5):488-91. [PubMed]
3. Jablonska S, Chorzelski T, Beutner E, Chorzelska J. Herpetiform pemphigus, a variable pattern of pemphigus. Int J Dermatol 1975;14:353-9. [PubMed]
4. Maciejowska E, Jablonska S, Chorzelski T. Is pemphigus herpetiformis an entity? Int J Dermatol 1987;26:571-7. [PubMed]
5. Binet O, Girard J, Beltzer-Garelly E, et al. Pemphigus herpetiform (spongiose a eosinophiles). Dermatologica 1979;159:151-9. [PubMed]
6. Crotty C, Pittelkow M, Muller SA. Eosinophilic spongiosis: a clinicopathologic review of 71 cases. J Am Acad Dermatol 1983;8:337-43. [PubMed]
7. Ishii K, Amagai M, Komai A et al. Desmoglein 1 and desmoglein 3 are the target autoantigens in herpetiform pemphigus. Arch Dermatol 1999;135:943-7. [PubMed]
8. Isogai R, Kawada A, Aragane Y, et al. A case of herpetiform pemphigus with anti-desmoglein 3 IgG autoantibodies. J Dermatol 2004;31(5):407-10. [PubMed]
9. Roux JS, Pascal F, Prost-Squarcioni C, et al. Pemphigus herpétiforme muqueux associé à une maladie de Basedow et à une recto-colite hemorragique. Ann Dermatol Venerol 2009 Dec;136:P198.
10. Braun-Falco O, Plewig G, Wolff HH, Burgdorf WHC. Blistering diseases. In: Braun-Falco O, Plewig G, Wolff HH, Burgdorf WHC, eds. Dermatology. 2nd, Completely Revised Edition. Berlin: Springer,2000,649-95.
11. Prado R, Brice SL, Fukuda S, Hashimoto T, Fujita M. Paraneoplastic pemphigus herpetiformis with IgG antibodies to desmoglein 3 and without mucosal lesions. Arch Dermatol. 2011;147(1):67-71. [PubMed]
12. Santi CG, Maruta CW, Aoki V, et al. Pemphigus herpetiformis is a rare clinical expression of nonendemic pemphigus foliaceus, fogo selvagem, and pemphigus vulgaris. J Am Acad Dermatol 1996;34:40-6. [PubMed]
13. Micali G, Musumeci ML, Nasca MR. Epidemiologic analysis and clinical course of 84 consecutive cases of pemphigus in eastern Sicily. Int J Dermatol 1998;37: 197-200. [PubMed]
14. Hamrouni I, Saidi W, Boussofara L, et al. Pemphigus herpétiforme: étude anatomo-clinique et évolutive (8 cas). Ann Dermatol Venerol 2009 Dec;136:P197.
15. Hocar O, Ouhajjou J, Akhdari N, Ait Sab I, Amal S. Un cas pédiatrique du pemphigus herpétiforme. Ann Dermatol Venerol 2009 Dec ;136 :F8.
16. Alison A. A case of pemphigus herpetiformis in a 10-year-old female. J Am Acad Dermatol 2009;60:AB145.
© 2011 Dermatology Online Journal

