Doxorubicin-induced hyperpigmentation
Published Web Location
https://doi.org/10.5070/D365m8x79pMain Content
Doxorubicin-induced hyperpigmentation
Naheed R Abbasi MD MPH, Nadia Wang MD
Dermatology Online Journal 14 (10): 18
Department of Dermatology, New York UniversityAbstract
A 39-year-old man with human immunodeficiency virus infection and Kaposi sarcoma on HAART therapy and doxorubicin presented in 2007 with a hyperpigmented tongue. Physical examination also showed hyperpigmented patches on the mucosal aspects of the lips and longitudinal dark bands on multiple nails. A skin biopsy specimen showed pigmentary alteration. Such hyperpigmentation has been described in numerous case reports and case series and has been reported to resolve within weeks to months of cessation of doxorubicin.
 |  |
| Figure 1 | Figure 2 |
|---|
History
A 39-year-old man with a history of human immunodeficiency virus infection and Kaposi sarcoma presented to the Dermatology Clinic at Bellevue Hospital Center in August, 2007, for evaluation of a dark tongue. The patient reported that his tongue had darkened over the prior three years. He also noted darkening of the mucosal aspect of his lips. While none of these changes was symptomatic, the patient was bothered by their cosmetic appearance.
Medical history includes a diagnosis of human immunodeficiency virus infection approximately five years ago and the development of Kaposi sarcoma three years ago. The patient had been treated with ritonavir, trizivir, and fosamprenavir for the past five years. Doxorubicin had been initiated for the treatment of Kaposi sarcoma approximately three years ago.
Physical Examination
A hyperpigmented plaque involved nearly the entire dorsal surface of the tongue and extended to the ventral aspect. Hyperpigmented brown patches were noted on the mucosal aspects of the lips. The fingernails and toenails also were noted to have longitudinal hyperpigmentation that affected multiple nails; numerous bands were noted on some nails.
Lab
A complete blood count and complete metabolic panel that included liver function tests were normal. A CD4 count of 759 cells and an viral load of <50 copies/ml were noted one month prior to presentation.
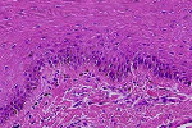
Histopathology
In the squamous mucosa, there is increased pigmentation of basilar keratinocytes and an increased number of melanophages in the lamina propria.
Comment
The association of chemotherapeutic agents with hyperpigmentation of the nails, mucosae, and skin has been reported for decades. In 1981, cutaneous effects of systemic cancer therapy were classified into three groups: cytotoxic effects, pigment alterations, and rashes and eruptions [1]. This classification has proved useful even in the context of novel chemotherapeutic agents that have been introduced in subsequent decades.
Many case reports and small case series dating back to the 1970s report the association of doxorubicin, an anthracycline antibiotic, with hyperpigmentation of the nails and skin. Hyperpigmentation of the nails and skin developed in 21 percent of 64 Chinese adults treated with doxorubicin alone or doxorubicin in combination with 5-fluorouracil and cyclophosphamide for various malignant conditions [2]. They reported fingernail and toenail hyperpigmentation as well as total cutaneous hyperpigmentation as possible side effects of the drug. Smaller case series and reports more specifically associate the use of doxorubicin with longitudinal bands and diffuse pigmentation of the fingernails, which resolves within weeks to months of discontinuation of therapy [3, 4]. Hyperpigmentation of the palms, soles, and buccal mucosa has been described [5, 6]. Hyperpigmentation of the tongue in two of ten children, who received doxorubicin for both solid and hematopoietic malignant conditions, occurred two weeks after initiation of drug [7].
Although the pathogenesis of doxorubicin-associated skin and nail hyperpigmentation has been postulated to be due to activation of melanocyte-stimulating hormone [8, 9], this hypothesis was not substantiated in two adults, in whom melanocyte stimulating hormone levels were measured [9]. Plasma cortisol levels were also normal in this analysis [9].
As in the patient we describe, skin biopsy specimens from previously reported patients with doxorubicin-associated hyperpigmentation are characterized by increased melanin deposition in the epidermis, particularly in the basal layer [2].
Although the resolution of skin and nail hyperpigmentation within weeks to months of discontinuation of doxorubicin has been described in numerous small case series [3, 4, 5, 6], drug cessation may not be feasible in some clinical contexts. The cosmetic impact of such pigmentation, particularly in its diffuse form, may be socially disabling [2].
References
1. Nixon DW, et al. Dermatologic changes after systemic cancer therapy. Cutis 1981; 27: 181, 186, 192 PubMed2. Alagaratnam TT, et al. Doxorubicin and hyperpigmentation. Aust N Z J Surg 1982; 52: 531 PubMed
3. Giacobetti R, et al. Nail hyperpigmentation secondary to therapy with doxorubicin. Am J Dis Child 1981; 135: 317 PubMed
4. Priestman J. Adriamycin and longitudinal pigmented banding of fingernails. Lancet 1975; i: 1337 PubMed
5. Law IP. Doxorubicin and unusual skin manifestations. Arch Dermatol 1977; 113: 379 PubMed
6. Rothberg H, et al. Adriamycin (NSC-123127) toxicity: unusual melanotic reaction. Cancer Chemother Rep 1974; 58: 749 PubMed
7. Rao SP, et al. Pigmentation of the tongue after treatment with adriamycin. Cancer Treat Rep 1976; 60: 1402 PubMed
8. Orr L, McKernan JF. Pigmentation with doxorubicin therapy. Arch Dermatol 1980; 116: 273 PubMed
9. Kew MC, Smith AG. Melanocyte-stimulating-hormone levels in doxorubicin-induced hyperpigmentation. Lancet 1977; i: 811 PubMed
© 2008 Dermatology Online Journal

