Hypomelanosis of Ito with hemimegalencephaly
Published Web Location
https://doi.org/10.5070/D36324c2wwMain Content
Hypomelanosis of Ito with hemimegalencephaly
Suvasini Sharma1, Naveen Sankhyan1, Madhulika Kabra2, Atin Kumar3
Dermatology Online Journal 15 (11): 12
1. Senior Research Associate, Division of Pediatric Neurology, Department of Pediatrics2. Incharge, Division of Genetics, Department of Pediatrics. madhulikakabra@hotmail.com
3. Assistant Professor, Department of Radiodiagnosis
All India Institute of Medical Sciences, New Delhi, India
Abstract
Hypomelanosis of Ito is a neurocutaneous syndrome characterized by hypopigmented lesions occurring in streaks and whorls located on the trunk, head or extremities. The associated neurological manifestations include mental retardation, seizures, language disabilities and motor system dysfunction. Hemihypertrophy has also been described in this syndrome. We present a 3-month-old male infant with Hypomelanosis of Ito, hemi-hypertrophy and hemi-megalencephaly.
Case report
A 3-month-old boy was brought for evaluation of developmental delay and seizures since 7 days of age. He was the second born child of a third degree consanguineous Muslim Indian couple. There was no history of toxin, medication, or radiation exposure during pregnancy and delivery at term was uneventful. Parents had noticed hypopigmented streaky lesions over the chest and back since birth. He developed focal seizures with tonic posturing of the right upper limb and deviation of his eyes to the left side on the seventh day of life. The frequency of seizures gradually increased from two to three per day to thirty per day by one month of age. Seizures were refractory to phenobarbital and phenytoin therapy. He had not achieved social smile or neck stability. Family history was non-contributory.
 |
| Figure 1 |
|---|
| Figure 1. Multiple streaky hypopigmented skin lesions (arrows) over the back of the child. |
Examination revealed a well-nourished infant with weight 5 kg, length 62 cm, and head circumference 40 cm. Discrete streaky hypopigmented macules with well defined margins were noted over chest and back (Fig. 1). Hemi-hypertrophy of left half of the body was present. The left lower limb was 2 cm longer than right lower limb (Fig. 2). Eye examination revealed lightly pigmented irises bilaterally, with normal fundi. Central nervous system examination revealed reduced alertness, reduced tone in all 4 limbs, brisk deep tendon reflexes, and extensor plantar response bilaterally. The rest of the systemic examination revealed no abnormalities. A clinical diagnosis of Hypomelanosis of Ito was made.
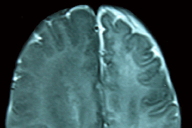
MRI of the brain revealed generalized enlargement of right cerebral hemisphere with cortical thickening consistent with hemimegalencephaly. (Fig. 3) Ultrasonography of abdomen was unremarkable.
Comments
Hypomelanosis of Ito (MIM 300337) is a neurocutaneous syndrome characterized by hypopigmented lesions occurring in streaks and whorls located on the trunk, head or extremities [1]. These skin lesions occur in all affected individuals and follow the lines of Blaschko. Other skin manifestations include café-au-lait spots, cutis marmorata, angiomatous nevi, nevus of Ota, dermal melanocytosis, hypohidrosis of hypopigmented areas, and morphea. Hair, tooth, and nail abnormalities can also occur. Hypomelanosis of Ito occurs sporadically and has been found to be associated with mosaicism for chromosomal abnormalities [2]. The pathogenesis of the disease is not well understood. Ultrastructural analysis shows decreased numbers of melanocytes, containing fewer melanosomes [3].
Common manifestations of central nervous system involvement include mental retardation, seizures, language disabilities, and motor system dysfunction. Abnormalities seen on brain imaging include hemi-megalencephaly, migrational abnormalities, agenesis of the corpus callosum, asymmetrical or symmetrical ventricular dilatation, focal cerebral atrophy with porencephalic ventricular dilatation, hemiatrophy, diffuse cerebral atrophy, cerebellar hypoplasia or atrophy, vascular abnormalities, and rarely tumors [4].
Hemi-megalencephaly consists of enlargement of one hemisphere of the brain with associated gyral malformations. Clinical features include early onset partial seizures (arising from the dysplastic hemisphere), hemiparesis, and hemianopia. Hemi-megalencephaly may occur as an isolated brain malformation or in association with neurocutaneous syndromes, as in the present case. These include linear nevus sebaceous syndrome, Klippel-Trenaunay syndrome, and neuromelanosis [5].
Hemihypertrophy has been described in 20 percent of patients with Hypomelanosis of Ito [1]. Patients with Hypomelanosis of Ito and hemi-megalencephaly often have unilateral skin lesions that are contralateral to the side of the brain malformation [6]. Our patient however had hemihypertrophy contralateral to the side of brain malformation, but skin lesions were distributed bilaterally on the trunk.
There is no treatment for the disorder, except for symptomatic management. The skin lesions require no special precautions or treatment. The hypopigmented lesions tend to darken with time. Individuals with seizures benefit from antiepileptic drugs, but almost 30 percent of patients have refractory epilepsy [7]. The lack of published series on the natural history of the disease makes accurate prognosis difficult. The presence of brain abnormalities in HMI appears to be associated with an enhanced frequency of neurological problems [4].
References
1. Pascual-Castroviejo I, Roche C, Martinez-Bermejo A, Arcas J, Lopez-Martin V, Tendero A, Esquiroz JL, Pascual-Pascual SI. Hypomelanosis of Ito. A study of 76 infantile cases. Brain Dev 1998 Jan;20(1):36-43. [PubMed]2. Sybert VP, Pagon RA, Donlan M, Bradley CM. Pigmentary abnormalities and mosaicism for chromosomal aberration: association with clinical features similar to hypomelanosis of Ito. J Pediatr 1990 Apr;116(4):581-6. [PubMed]
3. Vergine G, Mencarelli, Diomedi-Camassei F, Caridi G, Hachem ME, Ghiggeri GM, Emma F. Glomerulocystic kidney disease in hypomelanosis of Ito. Pediatr Nephrol 2008;23:1183-1187. [PubMed]
4. Tagawa T, Futagi Y, Arai H, Mushiake S, Nakayama M. Hypomelanosis of Ito associated with hemimegalencephaly: a clinicopathological study. Pediatr Neurol. 1997 Sep;17(2):180-4. [PubMed]
5. Gleeson GG, Dobyns WB, Plawner L, Ashwal S. Congenital structural defects. In: Swaiman KF, Ashwal S, Ferriero DM eds. Pediatric Neurology: Principles and practice. 4th Edition Mosby, Philadelphia: 2006; 363-490.
6. Iype M, Iype T, Geetha S, Retnakumar J. Hypomelanosis of Ito with cerebral malformation. Indian J Pediatr 2007 Nov;74(11):1044-5. [PubMed]
7. Oslon LL, Maria BL. Hypomelanosis of Ito. In Singer HS, Kossoff EH, Hartman AL, Crawford TO. Treatment of Pediatric Neurologic Disorders. Boca Ranton Taylor & Francis; 2005:561-564
© 2009 Dermatology Online Journal