Success of prednisone in the treatment of a patient with sarcoidosis and systemic sclerosis: Report of a case
Published Web Location
https://doi.org/10.5070/D362p1824wMain Content
Success of prednisone in the treatment of a patient with sarcoidosis and systemic sclerosis: Report of a case
João Borges da Costa, Augusto Mayer-da-Silva, Luís Miguel Soares de Almeida, Manuel Marques Gomes PhD
Dermatology Online Journal 15 (3): 11
Clínica Universitária de Dermatologia, Hospital de Santa Maria, Lisboa, Portugal. joaobc77@hotmail.comAbstract
We report a case of a man with sarcoidosis and diffuse systemic sclerosis who showed improvement of both diseases after prednisone therapy and remains asymptomatic after three years of follow-up. The association of these two diseases is rare and it is controversial whether this is a chance association or if there is a relationship between the two autoimmune diseases. Despite the poor prognosis and response to therapy of the patients with diffuse systemic sclerosis, our patient had a marked improvement of the disease with prednisone.
Introduction
The coexistence of sarcoidosis and diffuse systemic sclerosis (dSSc) is rare. This association may occur by chance; the two diseases may run independent clinical courses. However, it is also possible that the two may share some common immunopathogenic mechanism [1]. Some similarities in pathogenesis have been described that also include some findings in other granulomatous diseases, such as silicosis [2, 3]. Pulmonary involvement in these diseases may be especially difficult to differentiate.
Systemic sclerosis is a multisystem disorder of unknown etiology characterized by inflammatory, vascular, and sclerotic changes of the skin and various internal organs, with poor prognosis in its dSSc variant [4]. Most reports [3, 5] note the low efficacy of corticosteroid therapy in dSSc and in its association with sarcoidosis. We report a case with a good response.
Report of a case
Sarcoidosis was diagnosed in a 45-year-old male with a three to four year history of low grade fever and progressive dyspnea. Pulmonary biopsy revealed circumscribed granulomas of epithelioid cells with non-caseating necrosis.
In addition, computerized tomographic scans (CTS) revealed intrathoracic lymphadenopathy and pulmonary parenchymal changes. Pulmonary function tests demonstrated decreased carbon diffusing capacity, showing that the patient had interstitial lung disease with restrictive defects.
Treatment was initiated with 60 mg oral prednisone with progressive tapering. The patient was symptom free one year after the diagnosis.
Two years after the onset of sarcoidosis he had his first episodes of Raynaud phenomenon and one year later he developed cutaneous signs of systemic sclerosis. Pruritus, progressive hardening of the skin, leukoderma of the nape of the neck, trunk, perineum, forearms, and hands with perifollicular sparing, sclerodactyly, painful ulceration of fingertips, and limitation of wrist motion were then observed (Fig. 1).
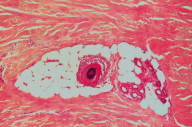
Biopsy of affected skin confirmed the clinical diagnosis of scleroderma (Fig. 2).
He had antinuclear antibodies (> 1/640), with an antinucleolar pattern of positivity, high titers of antibodies to topoisomerase I (Scl 70), and a twofold increase in erythrocyte sedimentation rate.
There was no evidence for internal organ involvement other than the pulmonary changes, which were unchanged from those previously seen with CT.
The patient was then again treated with oral prednisone (kept at 30 mg per day or less) for one year with progressive tapering, 400 mg oral pentoxifylline TID and 60 mg oral diltiazem BID.
 |  |
| Figure 3 | Figure 4 |
|---|---|
| Figure 3. Complete regression of leukoderma after one year of prednisone Figure 4. Regression of leukoderma and skin thickening of the hands | |
The frequency of his Raynaud phenomenon attacks was reduced and marked improvement of skin induration in all previously involved body areas was noted. There was complete regression of digital ulceration and leukoderma (Figs. 3 & 4). The wrist range-of-motion improved with exercise programs but residual sclerodactyly persisted.
The patient remains asymptomatic, with only rare episodes of Raynaud phenomenon during winter, three years after stopping prednisone. His current medications are diltiazem BID and pentoxifyline TID.
Comments
We present a man who developed systemic sclerosis two years after his diagnosis of sarcoidosis. Only a few cases of the association of these two diseases exist in the literature and in most of them the diagnoses were made simultaneously; in one case sarcoidosis was diagnosed more than 6 years after the onset of systemic sclerosis [5, 6].
Our patient had a good response to oral prednisone and remains asymptomatic in the three years of follow-up after stopping prednisone. Sarcoidosis associated with systemic sclerosis in two series of cases [3, 5] was reported to be more severe, persistent, and even associated with a poor response to oral corticosteroid therapy. However, in the oldest published series of cases of this association [6] there was an improvement of pulmonary symptoms with corticosteroid therapy.
Despite therapies available for dSSc, none has been shown to be of lasting benefit and no established guidelines for the management of patients with the association of sarcoidosis and systemic sclerosis are available. However, one prior patient had a successful response to the use of the endothelin receptor antagonist, bosentan [7]. We suggest that oral prednisone should not be underestimated in the management of these patients.
References
1. Enzenauer RJ, West SG. Sarcoidosis in autoimmune disease. Semin Arthritis Rheum. 1992; 22(1): 1-17. [PubMed]2. Takahashi T, Munakata M, Homma Y, Kawakami Y. Association of progressive systemic sclerosis with pulmonary Sarcoidosis. Just a chance occurrence? Intern Med. 1997; 36(6): 435-8. [PubMed]
3. M. de Bandt, S. Perrot, CH Masson, O. Meyer. Systemic Sclerosis and Sarcoidosis, a report of five cases. Br J Rheumatol. 1997; 36: 117-119. [PubMed]
4. Vincent Falanga. Systemic Sclerosis. In: Jean L Bolognia, Joseph L Jorizzo, Ronald P Rapini, eds. Dermatology. London: Mosby, 2003; vol 1(45): 625-630.
5. Bandt MD, Meyer O, Masson C, Peroux Goumy L, Audran M, Kahn MF. Systemic scleroderma and sarcoidosis: 3 new cases. Ann Med Interne (Paris). 1996; 147(8): 590-4. [PubMed]
6. Cox D, Conant E, Earle L et al. Sarcoidosis in systemic sclerosis: report of 7 cases. J Rheumatol.1995; 22:881-5. [PubMed]
7. Tillon J, Herve F, Chevallier D, Muir JF, Levesque H, Marie I. Br J Dermatol. 2006;154 (5):1000-2. [PubMed]
© 2009 Dermatology Online Journal