Exuberant cutaneous ulcers on the buttocks caused by multi-resistant
Published Web Location
https://doi.org/10.5070/D35fr811t1Main Content
Letter: Exuberant cutaneous ulcers on the buttocks caused by multi-resistant Klebsiella pneumoniae
Teresa Pinto-Almeida MD, Aristóteles Rosmaninho MD, Inês Lobo MD, Rosário Alves MD, Manuela Selores MD
Dermatology Online Journal 18 (8): 15
Department of Dermatology, Centro Hospitalar do Porto – Hospital de Santo António, Porto, PortugalAbstract
Cutaneous infection develops because of environmental and local factors, host immunity, and organism adherence and virulence. The authors report a case of exuberant cutaneous ulcers on the buttocks of a diabetic patient. Microbiologic examination allowed the identification of Klebsiella pneumoniae and complete resolution was achieved with the appropriate antibiotic.
Case report
An 83-year-old woman presented with painful cutaneous ulcers on the buttocks that developed over the previous 2 months. She denied trauma, application of irritant topical products, or other associated symptoms such as systemic or gastrointestinal symptoms. Her past medical history included chronic renal insufficiency, diabetes mellitus, and dyslipidemia for which she was on subcutaneous insulin and oral pravastatine. She was not bedridden and did not use diapers.
 |  |
| Figure 1 | Figure 2 |
|---|
Physical examination revealed well-circumscribed deep cutaneous ulcers, 2 on the left buttock and 2 on the right one, with suppurative exudative base and purulent discharge. The ulcers were surrounded by erythema and induration, measuring approximately 2-4 cm in diameter. She was afebrile and there was no lymphadenopathy. There were no other findings on physical examination.
Laboratory studies revealed leukocytosis (15.56 x 10³/μL, normal 4.00-11.00), neutrophilia (10.42 x 10³/μL, normal 2.00-7.50) and increased reactive C protein (98.02 mg/L, normal 0.0-5.0). The remainder of the laboratory tests, including serologies and immunology, were negative or within the normal range.
 |  |
| Figure 3 | Figure 4 |
|---|
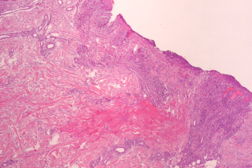
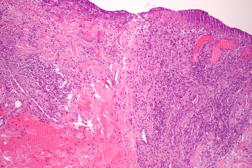
A skin biopsy from the edge of one ulcer was performed and histopathologic examination showed features of a nonspecific ulcer, with an inflammatory infiltrate at the base composed of lymphocytes, histiocytes, sparse neutrophils, and surrounding granulation tissue. Direct microbiologic examination of a skin biopsy revealed gram-negative bacilli and culture disclosed the growth of multi-resistant Klebsiella pneumoniae (extended-spectrum β-lactamase-producing strain), only sensitive to meropenem. Blood and urine cultures were negative.
 |  |
| Figure 5 | Figure 6 |
|---|
The patient started a 14-day course of IV meropenem 500 mg q12h (dose adjusted to renal function) with rapid improvement of the skin lesions.
Three weeks later, reepithelization of all the ulcers was complete and the patient remains free of lesions after one year of follow-up.
Discussion
The skin is a habitat for many commensal bacteria. Cutaneous infection develops because of environmental and local factors, host immunity, and organism adherence and virulence [1, 2]. Gram-negative organisms are not normally present on skin but may cause cutaneous infection [1, 2]. Diabetes mellitus is the most likely predisposing factor for the infectious ulcers in our patient, despite the uncommon localization [3]. We did not find in the indexed literature any report of Klebsiella skin infection on the buttocks. This fact highlights the importance of a high index of clinical suspicion. Microbiologic study of a skin fragment is essential for the correct diagnosis [4]. Dermatologists should be knowledgeable about this entity, playing a crucial role in early diagnosis and prompt treatment.
References
1. Berger TG. General considerations of bacterial diseases. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, eds. Fitzpatrick's Dermatology in General Medicine. 7th ed. The McGraw Hill Companies, Inc, 2008: 1689-93.2. Swartz MN. Gram-negative coccal and bacillary infections. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, eds. Fitzpatrick's Dermatology in General Medicine. 7th ed. The McGraw Hill Companies, Inc, 2008: 1741-3.
3. Varaiya AY, Dogra JD, Kulkarni MH, Bhalekar PN. Extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae in diabetic foot infections. Indian J Pathol Microbiol. 2008 Jul-Sep;51(3):370-2. [PubMed]
4. Eisenstein BI. Treatment challenges in the management of complicated skin and soft-tissue infections. Clin Microbiol Infect. 2008 Mar;17-25. [PubMed]
© 2012 Dermatology Online Journal

