Lymphomatoid Papulosis Localized to the Face
Published Web Location
https://doi.org/10.5070/D35ds430mgMain Content
Lymphomatoid papulosis localized to the face
Stéphane Dalle, Brigitte Balme, and Luc Thomas
Dermatology Online Journal 12 (3): 9
Service de Dermatologie, Hôpital de l’Hôtel-Dieu, 1 place de l’hôpital, 69288 Lyon Cedex 02. stephane.dalle@chu-lyon.frAbstract
We report a case of lymphomatoid papulosis (LyP) localized to the face. Only ten cases of localized LyP have been reported, and those involved the extremities. Three of those cases finally evolved to classic LyP with a widespread distribution of the lesions, the other cases remain limited. The evolution into lymphoma for the localized form appears to be equivalent to that reported with the generalized LyP (20 %), underlining the need for long-term followup of these patients. This is the first reported case of LyP localized to the face.
Lymphomatoid papulosis (LyP) is a disorder described by Macaulay in 1968 as a continuous self-healing, papular eruption, clinically benign and histologically malignant [1]. The disorder is characterized by erythematous papules and nodules that progress to form vesicular, crusted, or hemorrhagic lesions, and then undergo spontaneous healing with scarring. Lesions usually occur over the trunk and limbs. LyP is a usually benign cutaneous disease with alarming histopathology features. It is included among the cutaneous T-cell lymphomas in the recent WHO/EORTC classification of cutaneous lymphoma [2]. To the best of our knowledge eight cases of regional or localized LyP have been reported [3, 4, 5, 6, 7, 8], none with facial involvement.
Clinical synopsis
A 44-year-old man was referred to us in January 2005 for a 2-year history of a recurrent self-healing eruption limited to the right cheek. He was considered to have a chronic furunculosis or tinea barbae. However, neither topical nor systemic antibiotic or antimycotic therapy resulted in improvement. He noted occasional spontaneous healing of the eruption, usually following sun exposure during the summer.
On clinical examination he was noted to have an eruption of few reddish-brown papules ranging in diameter from 2 to 5 mm. These lesions became secondarily necrotic and painful. Only the right cheek was affected (Fig. 1); there were no similar lesions on trunk or limbs. The patient had no lymphadenopathy or hepatosplenomegaly. He was otherwise in good health, and his general examination was completely normal.
Peripheral blood count, liver function tests, renal function tests, and urinalysis were within normal limits. Myelogram and bone marrow biopsy were normal. Chest CT-Scan did not find mediastinal or abdominal lymphadenopathy.
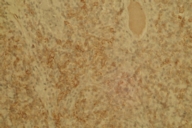
Histopathological examination of a skin biopsy taken from a cheek lesion revealed an epidermal hyperplasia and a dense infiltrate in the dermis with epidermotropism. This wedge-shaped infiltrate was composed of large atypical lymphocytes mixed with small lymphocytes, neutrophils, eosinophils, and histiocytes. Large atypical CD30+ cells did not form sheets and were fewer than 50 percent (Fig. 2). A few atypical mitoses could be seen. The atypical cells were stained by anti-CD4 and anti-CD30 antibodies. Few cells expressed CD8 and were interpreted as reactive lymphocytes. We did not detect a clonal rearrangement of the TCR-γ-chain gene.
We established, according to the recent WHO/EORTC classification on cutaneous lymphoma, the diagnosis of type-A LyP. Treatment with topical corticosteroid was followed by a rapid improvement of the lesions. At 12-months followup and 3 years after the beginning of the disease, the papules are still limited to the right cheek and controlled by topical treatment.
Regional involvement of LyP has been reported infrequently [3, 4, 5, 6, 7, 8, 9]. Eleven cases of regional LyP affecting the trunk or arms are reported in the English literature. Most of those cases are type-A LyP [4, 6, 9]. Three of the eleven patients eventually developed widespread lesions of typical LyP. Pediatric patients accounted for 25 percent of those reported [4, 6, 8]. Evolution to cutaneous T-cell lymphoma was noted in two patients (18 %), the same rate of evolution to malignancy expected for classic LyP. Although the etiology of localized LyP remains unknown, considering that 2 of 5 reported patients developed widespread lesions regional LyP may be the initial presentation of typical LyP [2, 7, 6, 9]. In a recent large retrospective study only one third of patients had a monoclonal TCR-γ rearrangement [9]. To the best our knowledge this is the first reported case of LyP localized to the face, although it is prudent to follow this patient closely for development of T-cell lymphoma.
References
1. Macaulay WL. Lymphomatoid papulosis. A continuing self-healing eruption, clinically benign--histologically malignant. Arch Dermatol 1968; 97: 23-30.2. Willemze R, Jaffe ES, Burg G et al. WHO-EORTC classification for cutaneous lymphomas. Blood 2005; 105: 3768-85.
3. Deroo-Berger MC, Skowron F, Ronger S et al. Lymphomatoid papulosis: a localized form with acral pustular involvement. Dermatology 2002; 205: 60-2.
4. Zirbel GM, Gellis SE, Kadin ME et al. Lymphomatoid papulosis in children. J Am Acad Dermatol 1995; 33: 741-8.
5. Kagaya M, Kondo S, Kamada A et al. Localized lymphomatoid papulosis. Dermatology 2002; 204: 72-4.
6. Scarisbrick JJ, Evans AV, Woolford AJ et al. Regional lymphomatoid papulosis: a report of four cases. Br J Dermatol 1999; 141: 1125-8.
7. Thomsen K, Hjort G, Svendsen D. Lymphomatoid papulosis. Dermatologica 1972; 144: 65-74.
8. Thomas GJ, Conejo-Mir JS, Ruiz AP et al. Lymphomatoid papulosis in childhood with exclusive acral involvement. Pediatr Dermatol 1998; 15: 146-7.
9. El Shabrawi-Caelen L, Kerl H, Cerroni L. Lymphomatoid papulosis: reappraisal of clinicopathologic presentation and classification into subtypes A, B, and C. Arch Dermatol 2004; 140: 441-7.
© 2006 Dermatology Online Journal