Erythematous nodule of the eyelid
Published Web Location
https://doi.org/10.5070/D35580173gMain Content
Erythematous nodule of the eyelid
Rym Benmously-mlika1, Elhem Khelifa1, Achraf Debbiche2, Hayet Marrak1, Mohamed ben Ayed2, Inçaf Mokhtar1, Samy Fenniche1
Dermatology Online Journal 14 (6): 14
1. Dermatology Department, Habib Thameur Hospital, Tunis, Tunisia. rym.benmously@rns.tn2. Anatomo-pathology Department, Habib Thameur Hospital, Tunis, Tunisia
Abstract
A 68-year-old woman had a 15-day history of a well-circumscribed, erythematous nodule of the left eyebrow/eyelid area. After excision a primary cutaneous large B-cell lymphoma was diagnosed. The tumor was excised with clear margins and the patient has shown no recurrence over two years.
Case Report
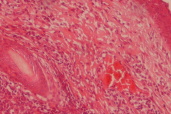
A 68-year-old woman presented with a 15-day history of a suddenly appearing and rapidly growing nodule of the left eyebrow/eyelid area (Fig. 1). The nodule measured 2x1 cm in size and was painful. There was no palpable lymphadenopathy. There was no history of trauma or insect bite. The rest of the skin had a normal appearance. Otherwise, she was asymptomatic and there was no recent deterioration in her health and the complete examination showed no lymphadenopathy.
 |  |
| Figure 1 | Figure 2 |
|---|---|
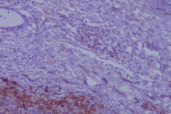
| Figure 1. Erythematous nodule of 2 cm diameter of the left eyelid Figure 2. Dense infiltrate of atypical lymphoid cells in the dermis without epidermotropism (HE x10) | |
At presentation, the nodule measured 2x1 cm in size (Fig. 1). The rest of the skin had a normal appearance. There was no deterioration in her health and the complete examination showed no lymphadenopathy.
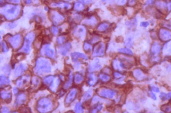
A biopsy from the nodule showed a dense infiltrate of atypical large lymphoid cells in the dermis with an overlying zone of uninvolved epidermis (Fig. 2). Immunohistochemically, the large atypical lymphoid cells stained positively for CD20 (Figs. 3 and 4).
 |  |
| Figure 3 | Figure 4 |
|---|---|
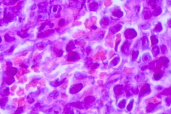
| Figure 3. Large atypical lymphoid cells, staining positively for CD20 Figure 4. Positivity of CD20 on higher magnification | |
The patient was admitted to our dermatology department. There was no evidence of lymphadenopathy on computed tomography scans of the chest, abdomen and pelvis. Analysis of the CBC and chemistries were normal and as was a bone marrow biopsy.
 |  |
| Figure 5 | Figure 6 |
|---|---|
| Figure 5. Proliferation of centroblasts and immunoblasts in the dermis (HEx30) Figure 6. Clinical aspect after surgical excision after a 2-year follow-up period. | |
Treatment with local radiation therapy was recommended, but refused by the patient. Therefore, complete surgical excision with clear margins was performed. The histological study showed a diffuse monotonous proliferation of centroblasts and immunoblasts (Fig. 5). Atypical cells also stained positive for CD79a and Bcl-2, typically found in primary cutaneous large B-cell lymphoma of the leg but absent in follicular center cell lymphoma of the head and trunk [1]. There were no recurrences after a 2-year follow-up period (Fig. 6).
Discussion
Approximately 27 percent of non-Hodgkin lymphomas occur in extranodal sites and the skin is the second most common site of extranodal involvement (18%), after the gastrointestinal tract [2]. Only 20-25 percent of primary cutaneous lymphomas are thought to originate from B cells [3]. Many classifications based on the histological aspect and the clinical localization are used. All demonstrated that the most common type of primary B-cell lymphoma of the head and neck is the follicle center cell lymphoma and that the diffuse large B-cell lymphoma is more frequent in the leg. We report in this study a rare case of primary cutaneous large B-cell lymphoma (leg-type) of the head.
A recent multicenter study documented that primary cutaneous large B-cell lymphomas with predominance of round cells, similar to our patient, have a worse prognosis than cases with predominance of large cleaved cells [4]. The estimated 5-year survival is about 72 percent; it is over 95 percent for other types of lymphomas of the head and neck [4]. In our patient, no recurrence was noted after a 2-year follow-up period.
For an isolated nodule, radiotherapy is the treatment of choice [5]. Some other studies evaluated the efficacy of rituximab, a monoclonal chimeric antibody targeting CD20 in the treatment of cutaneous B-cell lymphomas. The complete remission rate was about 25 percent and the partial remission rate about 56 percent [6, 7]. Our patient was treated by a complete surgical excision after refusing radiation therapy. Whatever classification and terminology is used by pathologists, fortunately, only a minority of patients with primary cutaneous B-cell lymphoma will die of their disease [8].
We reported this case for the rarity of diffuse large B-cell lymphoma of the head and its good prognosis in our patient.
References
1. Kerl H, Cerroni L. The morphologic spectrum of cutaneous B-cell lymphomas. Arch Dermatol 1996;132:1376-7. PubMed2. Groves FD, Linet MS, Travis LB, Devesa SS. Cancer surveillance series: Non-Hodgkin's lymphoma incidence by histologic subtype in the united states from 1978 through 1995. J Natl Cancer Inst 2000;92:1240-51.PubMed
3. Burg G, Kerl H, Przybilla B, Braun-Falco O. Some statistical data, diagnosis, and staging of cutaneous B-cell lymphomas. J Dermatol Surg Oncol 1984; 10: 256-62. PubMed
4. Grange F, Bekkenk MW, Wechsler J, Meijer CJLM, Cerroni L, Bernengo MG, et al. Prognostic factors in primary cutaneous large B-cell lymphomas: a European multicenter study. J Clin Oncol 2001;19:3602-10. PubMed
5. Santucci M, Pimpinelli N. Primary cutaneous B-cell lymphomas. Current concepts. I. Haematologica 2004;89:1360-1371. PubMed
6. Sabroe RA, Child FJ, Woolford AJ, Spittle MF, Russell-Jones R. Rituximab in cutaneous B-cell lymphoma ; a report of two cases. Br J Dermatol 2000;143:157-61.PubMed
7. Heinzerling LM, Urbanek M, Funk JO, Peker S, Bleck O, Neuber K et al. Reduction of tumor burden and stabilization of disease by systemic therapy with anti-CD20 antibody (Rituximab) in patients with primary cutaneous B-cell lymphoma. Cancer 2000;89:1835-44. PubMed
8. Slater DN. Primary cutaneous B-cell lymphoma: how useful is the new European Organisation for Research and Treatment of Cancer Classification? Br J Dermatol 1999;141:352-3; author reply 354. PubMed
© 2008 Dermatology Online Journal

