Coma blisters with hypoxemic respiratory failure
Published Web Location
https://doi.org/10.5070/D35175b1pgMain Content
Coma blisters with hypoxemic respiratory failure
Abhishek Agarwal MD1, Meghana Bansal MD1, Kelly Conner MD2
Dermatology Online Journal 18 (3): 10
1. Department of Internal Medicine2. Department of Dermatology
University of Arkansas for Medical Sciences, Little Rock, Arkansas
Abstract
A 24-year-old woman with quadriplegia was admitted with respiratory failure because of pneumonia. She was on multiple medications including diazepam, oxycodone, and amitriptyline, known to be associated with coma blisters, though she did not overdose on any of them. On hospital day 2, she developed multiple blisters on both sides of her right forearm and hand. Skin biopsy showed eccrine gland degeneration consistent with coma blisters. It was felt that hypoxemia from her pneumonia contributed to the development of these blisters, which occurred on both pressure and non-pressure bearing areas of the arm. Coma blisters are self-limited skin lesions that occur at sites of maximal pressure, mostly in the setting of drug overdose. However, coma blisters may occur with metabolic and neurological conditions resulting in coma.
Introduction
Coma blisters are self-limited skin lesions that occur at sites of pressure. They are most commonly associated with medication overdose, especially barbiturates, but may be seen in patients with coma from medical and neurological conditions. They may also be seen in non-comatose patients and in non-pressure bearing areas. We present a case of coma blisters occurring on both pressure bearing and non-pressure bearing areas of the right arm and hand.
A 24-year-old woman with traumatic quadriplegia and autonomic dysreflexia was admitted with altered mental status and shortness of breath. There was no history of recent fevers. Her home medications included diazepam, oxycodone, mirtazapine, and amitriptyline. On exam, she had a temperature of 37.6°C, respiration rate of 22 per minute, blood pressure of 116/84 and oxygen saturation of 86 percent on room air. She had coarse breath sounds over both lung fields. She had quadriplegia with contractures of the upper extremities. Laboratory findings were significant for an elevated white cell count of 18,000/mm³. Renal and hepatic function was normal. A chest X-ray showed multifocal infiltrates. She was intubated for airway protection and started on piperacillin-tazobactam for aspiration pneumonia.
 |
| Figure 1 |
|---|
| Figure 1. Multiple bullae lesions, some hemorrhagic, noted on both dorsal and ventral surface of distal arm. |
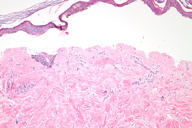
The patient was extubated within 24 hours of admission. On day 2, she was noted to develop multiple blisters on her right arm and hand. On skin exam, there were multiple well-demarcated, flaccid to tense intact bullae ranging in size from 5 mm to 4 cm on the patient's right palm, dorsal hand, wrist, and arm (Figure 1). Some of the bullae were hemorrhagic. Nikolsky sign was negative. The rest of the body was clear of bullae. The differential diagnosis included contact dermatitis, impetigo, bullous pemphigoid, and linear IgA disease. Bullous drug reaction was less likely because the lesions were focal.
 |  |
| Figure 2 | Figure 3 |
|---|---|
| Figure 2. Skin biopsy showing subepidermal bullae (H&E, x100) Figure 3: Skin biopsy showing early necrosis of eccrine sweat gland (H&E, x400) | |
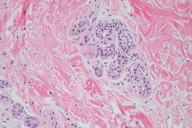
Histopathology showed a pauci-inflammatory subepidermal blister (Figure 2). There was no inflammatory infiltrate within the blister cavity or in the subjacent dermis. The eccrine glands showed degeneration (Figure 3). The vessels were not thrombosed. Direct immunofluorescence was negative. Given that there was no evidence of infection, drug reaction, autoimmune phenomenon or vasculopathy, the differential diagnosis included entities such as coma blister and suction blister.
The bullae on this patient had an unusual distribution on both sides of the arm and hand; coma blisters are usually found on pressure areas. There was no tight bandage around the arm, and though she was quadriplegic, the presence of blisters on both sides of the hand could not be explained by pressure alone. It was felt that hypoxemia contributed to the formation of the blisters.
Her pneumonia was successfully treated with a one-week course of piperacillin-tazobactam and she was weaned off supplemental oxygen. The skin lesions were conservatively treated with xerofoam gauze and kerlix wrap for comfort; she was discharged home on day 10 with continued dressings for the skin lesions. The lesions started to heal in 2 weeks and resolved in 3 weeks. No new lesions occurred during a 6-month follow up.
Discussion
Coma blisters are a self-limited cutaneous condition characterized by tense bullae that usually occur at sites of maximal pressure. They can occur in the setting of coma resulting from both drug and non-drug induced causes. Blisters typically develop 48-72 h after the onset of unconsciousness and heal spontaneously over 1 or 2 weeks [1]. Although barbiturates are most commonly reported with drug-induced coma blisters, benzodiazepines, opiates, tricyclic antidepressants, and antipsychotics have been reported as causative agents [2]. Bullae have also been observed in patients with coma resulting from chronic renal failure, hypercalcemia, diabetic ketoacidosis, and a variety of neurologic conditions [2].
The exact pathogenesis is still unclear, but may be related to hypoxia, pressure induced local ischemia, toxic effect of drugs on the skin and eccrine glands, and immune mechanisms [1]. Pressure-induced local ischemia seemingly leads directly to tissue injury proportional to the amount and duration of pressure. In the setting of uninterrupted pressure injury, arterial hypotension related to shock or vasoactive drugs may play a role [3]. Local anoxia causes a necrotic bulla and the typical selective destruction of the metabolically active cells such as eccrine sweat glands [4]. Amitriptyline is a highly lipophilic drug that has been shown to cause a dose-dependent decrease in transcellular resistance and increased endothelial cell permeability, which may increase susceptibility of the skin to blistering [5]. Although drug overdose is the most frequent predisposing event, lesions cannot be related specifically to the toxic effects of any medication [3]. Some studies suggest that immune mechanisms are also implicated in the pathogenesis of this condition [6]. Although the exact cause of coma blisters remains unknown, they are not related to underlying infections or rheumatologic disorders and do not contraindicate the continued use of any therapy [4].
The presence of characteristic skin lesions may be diagnostic in the appropriate setting, but histology can aid in the diagnosis. Histological findings include subepidermal bullae, focal necrosis of epidermis, dermis, subcutaneous tissue, and all epidermal appendages [3]. Eccrine sweat gland and sweat duct necrosis is the most remarkable and significant change, but its absence does not exclude the diagnosis [7]. The absence of inflammatory infiltrate in the epidermis and the presence of thrombosis in dermal vessels are the most important markers of non-drug-induced coma blisters [8]. Although the role of immunofluorescence studies in the biopsy specimen is not well established, there are studies that show deposits of immunoglobulins and/or complement in non-drug-induced coma blisters [6, 8, 9].
Similar pathologic findings have been reported in non-comatose patients and in non-pressure bearing areas [10]. Alterations of the sweat glands have also been described in other conditions such as neutrophilic eccrine hidradenitis, syringosquamous metaplasia, erythema multiforme, graft-vs-host disease, lichenoid dermatitis, toxic epidermal necrolysis, and vasculitis [10].
Etiology of these pathogenic lesions is broad and should be based on the clinical presentation. The management of the patient with coma blisters should take into account the benign nature of this condition, which is not related to any underlying infectious process and does not contraindicate continuation of any therapy [1]. The skin lesions usually resolve in 2 to 4 weeks, but early recognition and treatment of the underlying condition are crucial.
References
1. Rocha J, Pereira T, Ventura F, Pardal F, Brito C. Coma Blisters. Case Rep Dermatol. 2009 Oct 27;1(1):66-70. [PubMed]2. Piede J, Wallace E. Coma bullae: associations beyond medications. Mayo Clin Proc. 2011 Jan;86(1):e5. [PubMed]
3. Arndt KA, Mihm MC, Parrish JA. Bullae: a cutaneous sign of neurologic diseases. J Invest Dermatol. 1973;66:312-320. [PubMed]
4. Dunn C, Held JL, Spitz J, Silvers DN, Grossman ME, Kohn SR. Coma blisters: report and review. Cutis. 1990;45:423-426. [PubMed]
5. Maguiness S, Guenther L, Shum D. Coma blisters, peripheral neuropathy, and amitriptyline overdose: a brief report. J Cutan Med Surg. 2002 Sep-Oct;6(5):438-41. [PubMed]
6. Reiley CD, Harrington CI. Positive immunofluorescence in bullous lesions in drug-induced coma. Br J Dermatol. 1983;109:720-724. [PubMed]
7. Kim KJ, Suh HS, Choi JH, Sung KJ, Moon KC, Koh JK. Two cases of coma-associated bulla with eccrine gland necrosis in patients without drug intoxication. Acta Derm Venereol. 2002; 82:378-380. [PubMed]
8. Kato N, Ueno H, Mimura M. Histopathology of cutaneous changes in non-drug-induced coma. Am J Dermatopathol. 1996;18:344-350. [PubMed]
9. Arndt KA. Bullae in comatose and non-comatose patients. Acta Derm Venereol. 2003;83:236-237. [PubMed]
10. Ferreli C, Sulica VI, Aste N, Atzori L, Pinna M, Biggio P. Drug-induced sweat gland necrosis in a non-comatose patient: a case presentation. J Eur Acad Dermatol Venereol. 2003 Jul;17(4):443-5. [PubMed]
© 2012 Dermatology Online Journal

