Disseminated histoplasmosis presenting as panniculitis in two immunosuppressed patients
Published Web Location
https://doi.org/10.5070/D350j2g2r8Main Content
Disseminated histoplasmosis presenting as panniculitis in two immunosuppressed patients
Suzanne Quinter MD, C Lynn Cheng MD, Neha Prakash MD, Gabriel Currie MD, Matthew Fleming MD
Dermatology Online Journal 18 (11): 3
Medical College of Wisconsin, Milwaukee, WisconsinAbstract
We report two patients with polymyositis on immunosuppressive drugs and biologics with subsequent development of disseminated histoplasmosis presenting as panniculitis.
Introduction
Immunosuppressive drugs and biologics are common treatments for numerous dermatologic and rheumatologic conditions. The use of these medications, especially in combination, increases the risk of infection. Although histoplasmosis is usually asymptomatic or presents with only mild pulmonary symptoms, disseminated disease can occur in immunocompromised patients. Disseminated histoplasmosis is clinically heterogeneous and may be difficult to recognize. We present two patients with polymyositis treated with immunosuppressive drugs and rituximab who developed disseminated histoplasmosis presenting as panniculitis.
Case report 1
A 50-year-old female with an 11 year history of polymyositis was admitted to the hospital with complaints of subcutaneous nodules on the bilateral upper extremities. These had developed over the past 4 months, accompanied by increasing weakness and generalized pain. A review of systems was positive for fevers and chills, fatigue, malaise, blurry vision, dysphagia, shortness of breath, edema of the extremities, arthralgias, myalgias, backaches, easy bruising, and lymphadenopathy.
On admission, the patient was taking prednisone 40 mg daily and methotrexate 20 mg weekly. During the three months prior to her hospitalization, she had also received 2 infusions of rituximab 700 mg/m² (with a maximum of 1000 mg) one week apart as part of a clinical trial.
 |  |
| Figure 1A | Figure 1B |
|---|---|
| Figure 1. Erythematous, indurated, subcutaneous papules, and plaques were noted on the hands (1A), arms (1B), and back (1C). | |
 |
| Figure 1C |
|---|
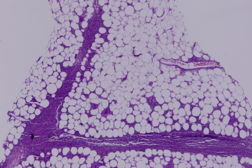
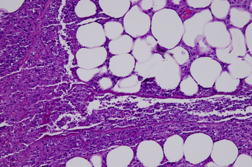
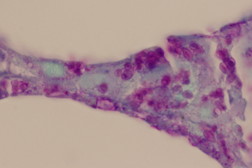
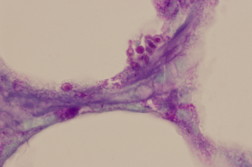
On physical exam, the patient had ill-defined, indurated, subcutaneous nodules and plaques with overlying erythema on the bilateral upper extremities and right back (Figure 1). Biopsy of a nodule on the left forearm demonstrated necrosis and dense neutrophilic inflammation in the subcutis (Figure 2). A few intracellular organisms, measuring approximately 4 μm/d, were visible in the subcutis in routinely stained sections. These organisms displayed the pseudocapsule characteristic of Histoplasma capsulatum. Many more organisms were visible in the subcutis in Gomori methenamine silver (GMS)- and Periodic acid-Schiff (PAS)-stained sections (Figure 3). Gram and acid fast bacillus (AFB) stains were negative.
 |  |
| Figure 2A | Figure 2B |
|---|---|
| Figure 2. Necrosis and a dense neutrophilic inflammation were noted in the subcutis (H&E x2 [2A], x10 [2B]). | |
 |  |
| Figure 3A | Figure 3B |
|---|---|
| Figure 3. Many organisms displaying the pseudocapsule characteristic of Histoplasma capsulatum were noted on Periodic acid-Schiff (x100 [3A] and [3B]). | |
Chest radiographs did not demonstrate active disease. Multiple blood cultures obtained throughout the hospital admission were negative. Both urine histoplasma antigen and blastomyces antigen were positive. CSF histoplasma antigen was also positive, indicative of central nervous system involvement.
The patient was treated initially with intravenous amphotericin B for 6 weeks followed by a one-year course of oral fluconazole.
Case report 2
A 53-year-old female with stable interstitial lung disease and a 25 year history of polymyositis was admitted to the hospital for a small, pink, tender nodule on her right upper arm. The patient denied fevers or chills on presentation, but a review of symptoms was positive for fatigue, shortness of breath, generalized pain, and weakness.
On admission, the patient was taking 20 mg prednisone and 150 mg azathioprine daily. She had also been previously enrolled in a rituximab trial in which she received two doses of 700 mg/m² (with a maximum of 1000 mg) one week apart. Physical examination showed a 6 cm bright pink, indurated, tender, warm plaque with erythema extending circumferentially measuring 15 cm in diameter. The lesion was initially treated as a cellulitis with several courses of antibiotics, but the plaque did not resolve. After clinical worsening, eruption of new plaques and ulceration of older plaques two skin biopsies were taken. The biopsies demonstrated a mixed lobular and septal granulomatous infiltration of the subcutis. PAS and AFB stains were negative.
Fungal, mycobacterial and bacterial cultures, urine histoplasmosis antigen, TB PCR and serum Quantiferon were all negative at that time.
CT of the chest was negative for pulmonary nodules, consolidations, or lymphadenopathy. With infectious tests negative, further treatments for erythema nodosum were pursued including increased prednisone, hydroxychloroquine, supersaturated potassium iodide (SSKI), mycophenolate mofetil, colchicine, and dapsone all of which were ineffective in reducing the skin lesions.
Over the following 10 months, the disease progressed to 10 lesions, some with central ulceration, all ecchymotic and indurated, ranging from 4 to 20 cm in diameter, scattered across both arms, left leg, abdomen, and buttocks. A second incisional biopsy of the left thigh suggested panniculitis-like alpha-beta T cell lymphoma with CD3+, CD8+, TIA1+, CD4-, CD56-, CD30-, EBER- immunohistochemistry. However, repeat tissue culture eventually grew histoplasmosis. Repeat urine histoplasmosis antigen was subsequently positive at that time as well. The patient was immediately admitted for IV Amphotericin B for 2 weeks and was discharged with dramatic improvement. The patient completed a year course of oral itraconazole with resolution of symptoms and skin lesions.
Discussion
Histoplasmosis is caused by the dimorphic fungus Histoplasma capsulatum. Although worldwide in distribution, Histoplasma is most prevalent in the Southeast and Central US. In endemic areas, over half of adults have been infected. Initial infection occurs with inhalation of the spores, followed by hematogenous dissemination during the first 2 weeks. Cellular immunity subsequently suppresses the infection as CD4+ T-cells and activated macrophages acquire fungicidal activity [1]. Humoral immunity, although classically not considered as integral in anti-fungal defense, does likely influence and promote T-cell anti-fungal activity [2].
In immunologically intact hosts, histoplasmosis is usually asymptomatic. Less than 5% of exposed individuals will develop symptomatic disease after low-level exposure. Among the patients who do develop symptoms, common manifestations include a flu-like pulmonary illness, pericarditis, or arthritis with erythema nodosum [3]. Although rare, disseminated histoplasmosis can also occur, especially in the setting of an immune deficiency or in the very young or old. It can present as an acute, rapidly fatal disease with diffuse reticuloendothelial involvement. Alternatively, as demonstrated in the presented cases, disseminated histoplasmosis can run a more chronic, slowly progressive course, with fever, night sweats, anorexia, weight loss, fatigue, and respiratory symptoms [1].
Various skin lesions have been described in disseminated histoplasmosis. Oropharyngeal ulcerations are the most common mucocutaneous manifestation. Lesions begin as flat, non-tender plaques or nodules that evolve into painful ulcerations. Other reported skin findings include indurated, erysipelas-like plaques with ulceration nodules that progress to ulcers with heaped up margins and subcutaneous, painless erythema nodosum-like nodules [4].
There are only a few previous case reports of Histoplasma panniculitis [5, 6, 7, 8]. In all cases, the lesions appeared clinically as erythematous, indurated plaques and were a manifestation of disseminated disease. In almost all the cases, the patients were immunocompromised, usually as a result of immunosuppressive therapy for a connective tissue disease such as dermatomyositis, systemic lupus erythematosus, or rheumatoid arthritis. The reported immunosuppressives medications include prednisone, methotrexate, leflunomide, mycophenolate mofetil, azathioprine, and infliximab [5, 6, 7, 8].
There are also case reports of histoplasmosis associated with rituximab therapy. In one study, lupus nephritis refractory to conventional therapy was treated with rituximab. In this series, 1 of the 22 patients died because of invasive histoplasmosis, massive pulmonary hemorrhage, and mucormycosis. In addition to rituximab, the patient was simultaneously receiving 3 additional immunosuppressive medications and high doses of glucocorticoids [9]. In another study of patients awaiting renal transplantation who received rituximab for reduction of anti-HLA antibodies, 1 of the 9 patients developed presumed histoplasmosis with chest pain and shortness of breath that resolved with empiric itraconazole therapy [10].
Similar to the reported cases discussed above, our cases occurred in two patients receiving multiple immunosuppressive drugs. Whereas the diagnosis of histoplasmosis was reached quickly in the first case, the second case had a delayed diagnosis. The delay stemmed from the organisms not being readily identified on skin biopsy, but also by a delayed positive tissue culture and urine histoplasma antigen test. By the time the final and correct diagnosis was reached, the patient had undergone three urine histoplasma antigen tests and two fungal skin cultures. Interestingly, the other diagnoses that were being considered were broad and included erythema nodosum early in the disease course and a rare, panniculitic-like T cell lymphoma later in the disease course. This highlights how inflammatory infiltrates of fungal infections can mimic many other entities histologically. Importantly, an infectious cause was continually pursued while entertaining the other diagnostic possibilities.
In an era of widespread immunosuppressive therapy and increasing use of biologics, it is important to recognize atypical presentations of potentially life-threatening, disseminated infections. As shown in our cases, panniculitis is one such presentation, which should be kept in mind.
References
1. Wheat LJ, Kauffman CA. Histoplasmosis. Infect Dis Clin North Am. 2003 Mar; 17(1): 1-19, vii. Review. [PubMed]2. Romani, L. Immunity to Fungal Infections. Nature Reviews Immunology. 2004 Jan: 4: 11-24. Review. [PubMed]
3. Wheat J. Histoplasmosis. Experience during outbreaks in Indianapolis and review of the literature. Medicine (Baltimore). 1997 Sep; 76(5):339-54. Review. [PubMed]
4. Goodwin RA Jr, Shapiro JL, Thurman GH, et al. Disseminated histoplasmosis: clinical and pathologic correlations. Medicine (Baltimore). 1980; 59:1-33. [PubMed]
5. Bhowmik D, Dinda AK, Xess I, Sethuraman G, Mahajan S, Gupta S, Agarwal SK, Guleria S, Tiwari SC. Fungal panniculitis in renal transplant recipients. Transpl Infect Dis. 2008 Jul;10(4):286-9. Epub 2007 Dec 11. [PubMed]
6. Ceccato F, Gongora V, Zunino A, Roverano S, Paira S. Unusual manifestation of histoplasmosis in connective tissue diseases. Clin Rheumatol. 2007 Oct;26(10):1717-9. Epub 2007 Jun 1. [PubMed]
7. Sawalha AH, Lutz BD, Chaudhary NA, Kern W, Harley JB, Greenfield RA. Panniculitis: a presenting manifestation of disseminated histoplasmosis in a patient with rheumatoid arthritis. J Clin Rheumatol. 2003 Aug;9(4):259-62. [PubMed]
8. Silverman AK, Gilbert SC, Watkins D, Cooper B, Menter A. Panniculitis in an immunocompromised patient. J Am Acad Dermatol. 1991 May;24(5 Pt 2):912-4.
9. Abildgaard WH Jr, Hargrove RH, Kalivas J. Histoplasma panniculitis. Arch Dermatol. 1985 Jul;121(7):914-6. [PubMed]
10. Vigna-Perez M, Hernández-Castro B, Paredes-Saharopulos O, Portales-Pérez D, Baranda L, Abud-Mendoza C, González-Amaro R. Clinical and immunological effects of Rituximab in patients with lupus nephritis refractory to conventional therapy: a pilot study. Arthritis Res Ther. 2006;8(3):R83. Epub 2006 May 5. [PubMed]
© 2012 Dermatology Online Journal

