Primary ecthyma gangrenosum as a presenting sign of leukemia in a child
Published Web Location
https://doi.org/10.5070/D34tm8z0ggMain Content
Primary ecthyma gangrenosum as a presenting sign of leukemia in a child
Matthew Fink BS1, Dennis Conrad MD2, Mark Matthews MD3, John C Browning MD1,2
Dermatology Online Journal 18 (3): 3
1. Division of Dermatology and Cutaneous Surgery, University of Texas Health Science Center at San Antonio, San Antonio, Texas2. Department of Pediatrics, University of Texas Health Science Center at San Antonio, San Antonio, Texas
3. Christus Santa Rosa Children’s Hospital, San Antonio, Texas
Abstract
Ecthyma gangrenosum is a type of skin infection characterized by black eschars on an erythematous base. It most commonly occurs with pseudomonas infection in an immunocompromised setting. We present a case of primary ecthyma gangrenosum as the presenting sign of pre-B acute lymphoblastic leukemia (ALL) in a child.
Case report
A 5-year-old boy with a past medical history significant for trisomy 21 and tetralogy of Fallot that was repaired at 4 months of age, presented to the emergency center with painful, black skin lesions on his chest. The patient’s mother stated that he had been febrile over the last several days and that the sores on his chest were initially small and red and then progressed to bumps that ulcerated and darkened. She denied the presence of any similar lesions on family members with whom the child lives. The child also presented with reduced appetite, nausea, vomiting, and a history of a loose bowel movement.
 |  |
| Figure 1 | Figure 2 |
|---|
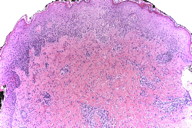
Physical examination revealed a fussy child with six lesions located on the trunk ranging from 1.5 cm to 2 cm in diameter. Each raised plaque exhibited an area of black, necrotic-appearing central depression with a rim of erythema and surrounding petechiae. No regional lymphadenopathy was noted. On admission, laboratory values were significant for WBC 1000/mm³, hemoglobin and hematocrit 6.4 g/dl and 18.6 percent, respectively, platelets 15,000/mm³, ANC 380, lymphocytes 50 percent, blasts 3 percent. Albumin and total protein were 2.4 g/dl and 5.9 g/dl respectively and the coagulation profile revealed slightly elevated PT, INR, PTT, and fibrinogen at 15.5 seconds, 1.26, 30.9 seconds, and 546 MG percent.
Subsequent to hospital admission, the child was diagnosed with pre-B ALL and induction therapy was begun. Blood cultures from the transferring institution were negative. Diagnosis was made by way of wound culture.
Skin biopsy sent for tissue culture grew colonies of Pseudomonas aeruginosa, but blood cultures on three different days never showed any growth.
The child was placed on ceftazidime and subsequently all cutaneous lesions healed. He continues to do well and has started chemotherapy without any complications.
Discussion
Clinically, ecthyma gangrenosum most frequently presents as hemorrhagic bullae or necrotic ulcers that have progressed from painless macules or papules. Often the presenting lesion will exhibit an erythematous halo. Depending on the extent of infection and immune status, the patient may also be febrile with other constitutional symptoms. Diarrhea and gastrointestinal upset are also commonly associated symptoms [1, 2, 3].
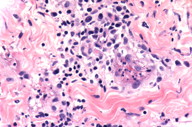
Histologic findings are characterized by necrotizing vasculitis in which the media and adventitia of the vascular wall are invaded, but the intima is spared [2]. This manner of precipitating vasculitis is distinctive from other bacterial species that demonstrate proclivity for vessel invasion in which bacteria, carried through the vasculature, attach to intraluminal thrombi and penetrate the endothelium first [6]. Several virulence factors, including elastase, alkaline protease, and endotoxin A, facilitate vascular involvement and ensuing tissue necrosis [2].
 |  |
| Figure 3 | Figure 4 |
|---|
Whereas well-developed lesions of ecthyma gangrenosum are reportedly characterized by numerous Gram-negative bacterial rods within the dermis between the collagen bundles and in the media and adventitia of small blood vessels, earlier lesions may show few if any bacteria detectable by staining technique. However, tissue resident bacteria such as Pseudomonas aeruginosa, typically remain detectable by lesion culture technique. The current biopsy shows changes suggestive of an earlier ecthyma gangrenosum lesion with epidermal spongiosis and a mixed dermal infiltrate composed of lymphocytes, histiocytes, and granulocytes (Figure 3). Closer inspection also demonstrates the infiltrate to be interstitial and angiocentric with some small caliber vessels revealing changes of early necrotizing vasculitis (Figure 4). A spectrum of vasculopathic and tissue changes, from frank tissue necrosis with accompanying well-developed necrotizing vasculitis to early dermal mixed infiltrate with early vasculitis changes, may be encountered depending upon the evolutionary stage of the biopsied lesion.
Pseudomonas aeruginosa is a robust pathogen that flourishes in water and is capable of surviving extremes of temperature as well as antiseptics. Colonization most frequently occurs in the gastrointestinal tract and can spread to the axillae and perineum [1]. The lesions of ecthyma gangrenosum are most commonly found in the anogenital region, buttocks, extremities, and abdomen [2].
Although it can be caused by other bacterial and fungal species (Staphylococcus aureus, Aeromonas hydrophila, Serratia marcescens, Aspergillus spp., Candida spp., Fusarium spp., and Rhizopus) ecthyma gangrenosum most commonly results from pseudmonal bacteremia [6]. This pseudomonal bacteremia frequently occurs in the setting of immunocompromise, in which the risk of disseminated infection is particularly high, such as in cases of neutropenia with a granulocyte count < 1.0 x 109 [4]. Healthy infants without evidence of immune deficiency have also been found to be at increased risk of pseudomonal bacteremia [1].
Whereas it is uncommon to see it in the absence of bacteremia, ecthyma gangrenosum can present as a primary skin infection as well, as occurred in this case. Interestingly, there is an association in the literature between acute lymphoblastic leukemia and primary ecthyma gangrenosum (pseudomonal skin infection in the absence of bacteremia) [6]. It is likely that primary ecthyma gangrenosum is associated with skin changes commonly found in children being treated for ALL or suffering from neutropenia. These changes include shifts in skin flora, alterations in the stratum corneum, and increased hydration and humidity on the epidermal surface [6]. As is the case with several other species, which infect immunocompromised patients, ecthyma gangrenosum secondary to primary skin infection by P. aeruginosa can precede the onset of hematologic malignancies [6]. In fact, there is a potential association between ecthyma gangrenosum, in the absence of bacteremia, and later diagnosis of ALL [5]. It is hypothesized that transient neutropenia, known to manifest prior to lymphoblastosis, facilitates infection with opportunistic pathogens [5].
Outcomes for patients in whom pseudomonal infection has precipitated ecthyma gangrenosum in the absence of bacteremia are significantly better than in those patients afflicted with cutaneous manifestations of septicemia. Various authors cite mortality rates from 38 percent to 70 percent in cases of P. aeruginosa septicemia and from zero to 28 percent in cases of skin lesions without bacteremia [1, 2, 5, 6]. Work-up should include a CBC with differential, CMP, albumin, total protein, and immune deficiency evaluation. Predictably, treatment consists of antimicrobials active against pseudomonal species including ciprofloxacin and IV cefepime, ceftazidime and gentamicin, piperacillin/tazobactam.
Although ecthyma gangrenosum can occur in patients with pseudomonas bacteremia in spite of negative blood cultures, we believe our case to be consistent with primary ecthyma gangrenosum. This is supported by the patient’s quick response to ceftazidime and favorable clinical outcome.
References
1. Fergie J, Patrick C, Lott L. Pseudomonas aeruginosa cellulitis and ecthyma gangrenosum in immunocompromised children. Ped Infect Dis. 1991; 10: 496. [PubMed]2. Pouryousefi A, Foland J, Michie C, Cummins M. Ecthyma gangrenosum as a very early herald of acute lymphoblastic leukemia. J Ped Health. 1999; 35: 505. [PubMed]
3. Fergie J, Shema S, Lott L, Crawford R, Patrick C. Pseudomonas aeruginosa bacteremia in immunocompromised children: analysis of factors associated with a poor outcome. Clin Infect Dis. 1994; 18: 390 [PubMed]
4. Singh T, Devi KM, Devi KS. Ecthyma gangrenosum: a rare cutaneous manifestation caused by pseudomonas aeruginosa without bacteremia in a leukemic patient – a case report. Indian J of Med Micro. 2005; 23: 262. [PubMed]
5. Gencer S, Ozer S, Gul AE, Dogan M, Ak O. Ecthyma gangrenosum without bacteremia in a previously healthy man: a case report. J of Med Case Rep. 2008; 2: 14. [PubMed]
6. Chan YH, Chong CY, Puthucheary J, Loh TF. Ecthyma gangrenosum: a manifestation of Pseudomonas sepsis in three pediatric patients. Singapore Med J. 2006; 47: 1080. [PubMed]
© 2012 Dermatology Online Journal

