Subcutaneous midline suprasternal mass in a ten-month-old girl
Published Web Location
https://doi.org/10.5070/D34tc9658pMain Content
Subcutaneous midline suprasternal mass in a ten-month-old girl
Margarita Larralde MD PhD1, Ana Isabel Sánchez Moya MD2, Maria Eugenia Abad MD1, Paula C Luna MD1, Fernando Heinen MD3, Gabriel Casas MD4
Dermatology Online Journal 16 (6): 6
1. Pediatric Dermatology Department, Ramos Mejía Hospital, Buenos Aires, Argentina2. Department of Dermatology, Complejo Hospitalario Toledo, Spain. anai.sanchezmoya@yahoo.es
3. Paediatric Surgeon Department, Aleman Hospital, Buenos Aires, Argentina
4. Department of Histopathology, Aleman Hospital, Buenos Aires, Argentina
Abstract
A ten-month-old girl presented to our clinic with a progressively enlarging congenital mass at the midline suprasternal location. Histopathologic examination revealed a benign cyst with stratified squamous keratinized epithelium with numerous eccrine glands in the sinus wall. The diagnosis was compatible with dermoid cyst. Dermoid cysts of the trunk are rare lesions, but a midline location is characteristic for these congenital masses. A dermoid cyst should be high on the list of differential diagnoses given a unilocular midline cyst in a neonate.
Case report
A ten-month-old healthy girl was referred to our department for evaluation of a subcutaneous midline suprasternal mass. Her parents reported that the lesion was present since birth and there were no episodes of inflammation or infection. Physical examination showed a soft, subcutaneous, skin colored mass with a central bluish depression. She was otherwise healthy and asymptomatic (Figure 1). Ultrasonography revealed a subcutaneous, well-defined cyst with a homogenous content. There were no septations or calcifications and it measured 19 x 10 mm without extension to adjacent soft-tissue structures. Doppler examination showed lack of blood flow.
The patient was lost to follow-up until three years later. A new ultrasonography disclosed a 46 x 15 x 30 mm mass with the same previous echographic characteristics (Figure 1). Under general anesthesia, the intact mass was enucleated. The external surface was smooth, pink-tan and translucent (Figure 2). The postoperative course was uneventful.
 |  |
| Figure 1 | Figure 2 |
|---|
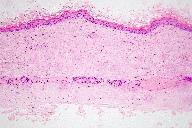
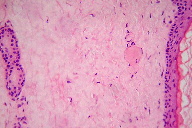
Histopathologic examination revealed a benign cyst with stratified squamous keratinized epithelium (Figure 3). Numerous eccrine glands were observed next to and in the sinus wall (Figure 4). The lesion was histologically diagnosed as a dermoid cyst.
 |  |
| Figure 3 | Figure 4 |
|---|
Discussion
Dermoid cysts may be classified as congenital or acquired. Acquired cysts are derived from traumatic or iatrogenic inclusions of epithelial cells or from the occlusion of a duct. Congenital dermoid cysts can occur anywhere in the body at an embryologic fusion point; these may be classified into four categories based on location and corresponding embryogenesis [1]. Group 1, the most common, is periorbital in the region of the embryologic maxillary and mandibular processes at the naso-optic groove. Group 2 are seen at the bridge of the nose near the frontonasal plate. Group 3 are submental, floor of the mouth, or thyrohyoidal, where the first and second branchial arches fuse in the midline. The case we present fits into the group 4. These are seen at mid-ventral or mid-dorsal embryologic fusion sites, either thyroidal, suprasternal or suboccipital [1, 2, 3].
Although dermoid cysts of the anterior chest region are rare [2, 4, 5, 6] these should be included in the differential diagnosis of midline suprasternal cysts. This includes thyroglossal duct cyst, epidermoid cyst and thymic cyst. Bronchogenic cysts have been reported at the suprasternal notch, although this is an unusual location [7, 8]. In this location epidermoid cysts are more frequent than dermoid cysts [4]. The embryological theory proposed is that the primitive epithelium has a high capacity to differentiate. Therefore, in the early stages of inclusion, they can give rise to both dermoid and epidermoid cysts. However, if the inclusion happens later on, it will result in epidermoid cysts only [1].
That is why histologically, dermoid cysts entirely reproduce the features of the normal skin. They are composed by a cavity filled with keratinous material and lined by stratified squamous epithelium comprising hair follicles, sebaceous glands, and more rarely, sweat glands.
Presurgical imaging of these lesions is important to evaluate for any evidence of extension to periosteum or adjacent structures that may impact on surgical removal [9].
Surgery is the only effective treatment for these lesions. The whole lesion should be excised, including its capsule, to avoid the recurrence. Prognosis is usually excellent with almost no recurrence being reported.
We suggest that even asymptomatic lesions should be excised to prevent infection and confirm diagnosis. In addition fairly early surgery is advised because of the tendency to grow to great size, complicating surgical excision.
References
1. McAvoy JM, Zuckerbraun L. Dermoid cysts of the head and neck in children. Arch Otolaryngol 1976;102(9): 529-31. [PubMed]2. Vittore CP, Goldberg KN, McClatchey KD et al. Cystic mass at the suprasternal notch of a newborn: congenital suprasternal dermoid cyst. Pediatr Radiol 1998; 28(12):984–86. [PubMed]
3. Görür K, Talas DU, Ozcan C. An unusual presentation of neck dermoid cyst. Eur Achr Otorhinolaryngol 2005;262(4):353-355. [PubMed]
4. Yilmaz M, Vayvada H, Demirdöver C. Dermoid cyst at the suprasternal notch. Ann Plast Surg 2000; 45:343. [PubMed]
5. Savranlar A, Ozer T, Numanoğlu V, Gün BD. Radiologic findings of a congenital suprasternal dermoid cyst. Kulak Burun Bogaz Ihtis Derg. 2005;14(5-6):131-4. [PubMed]
6. Zhang XY, Ishihara T, Ono T. Dermoid cyst at the suprasternal notch: an adult case. Scand J Plast Reconstr Surg Hand Surg 2005;39(1):57-9. [PubMed]
7. Turkyulmaz Z, Karabulut R, Bayazit YA, et al. Congenital neck masses in children and their embryologic and clinical features. B-ENT 2008;4(1):7-18. [PubMed]
8. Shah SK, Stayer SE, Hicks MJ, Brandt ML. Suprasternal bronchogenic cyst. J Pediatr Surg 2008;43(11):2115-7. [PubMed]
9. Teixeira RL, Lacerda MB, Paim NP. Gigant dermoid cyst of sternum. Cir Pediatr. 2007:20(4):232-33 [PubMed]
© 2010 Dermatology Online Journal

