Cutaneous Rosai-Dorfman disease
Published Web Location
https://doi.org/10.5070/D34rd8h0gsMain Content
Cutaneous Rosai-Dorfman disease
Joseph F Merola MD, Melissa Pulitzer MD, and Karla Rosenman MD, Isaac Brownell MD PhD
Dermatology Online Journal 14 (5): 8
Department of Dermatology, New York UniversityAbstract
A 63-year-old woman developed multiple nodules at the site of a recently biopsied mass showing proliferation of CD 68+ histiocytes. Clinical lymphadenopathy was not present on physical examinaton or on computed tomography scans. A subsequent skin biopsy specimen showed changes consistent with Rosai-Dorfman disease. Rosai-Dorfman disease is a benign, histiocytic proliferative disorder also known as sinus histiocytosis with massive lymphadenopthy. A particularly rare, extranodal, purely cutaneous form has been described. Spontaneous regression tends to occur over months to years, with surgical intervention remaining the most effective treatment. Successful treatment has been documented with a number of other therapies which include systemic high-dose thalidomide in extensive cutaneous disease.
Clinical synopsis
A 63-year-old woman was referred to the Dermatology Clinic at Bellevue Hospital Center for evaluation of progressively enlarging skin lesions that were adjacent to a biopsy scar. In August 2005 the patient was evaluated at another hospital for a superficial soft tissue mass that was increasing in size over the course of 3 months. That November an excisional biopsy demonstrated a proliferation of CD68+ histiocytes. No lymphadenopathy was noted. Approximately 5 months later, an erythematous patch developed near the biopsy scar, which became progressively more nodular in quality. The patient's past medical history includes hypertension, osteoporosis, breast cancer (diagnosed in 1989, status-post right mastectomy and chemotherapy), and sarcoidosis (diagnosed in 1976 by lung biopsy). The patient denied fevers, chills, or weight loss. Medications include atenolol and risedronate.
Physical examination
 |
| Figure 1 |
|---|
Multiple, red-brown nodules with translucent yellow centers that ranged in size from 1 to 3 cm as well as two subcutaneous nodules were present adjacent to a linear scar on the right thigh. The patient was afebrile; cervical, supraclavicular, axillary, inguinal lymphadenopathy, and hepatosplenomegaly were absent.
Laboratory data
Complete blood count, liver function tests, and basic metabolic panel were normal. Serum protein electrophoresis demonstrated no gammopathy. A computed tomography scan of chest, abdomen, and pelvis in March 2006 did not show lymphadenopathy. A benign-appearing cystic expansile lesion was noted in the right pelvis.
Histopathology
 | 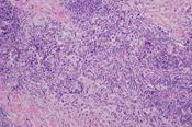 |
| Figure 2 | Figure 3 |
|---|
There is a nodular, mixed-cell infiltrate of histiocytes, lymphocytes, and plasma cells with a few scattered multinucleated cells. There are scattered, enlarged S-100+ histiocytes that contain plasma cells and lymphocytes within their cytoplasm. A stain for CD1a is negative.
Comment
Rosai-Dorfman disease (RDD) was first described by Destombes in 1965 [1] and then recognized as a distinct entity in 1969 by Rosai and Dorfman [2]. This histiocytic, proliferative disorder, which also is known as sinus histiocytosis with massive lymphadenopthy, usually presents with lymphadenopathy in children or young adults. The condition is more predominant in men and has been reported in both blacks and whites. This disorder is usually non-progressive and self-limited. Patients may manifest an autoimmune hemolytic anemia [3]. Fever, leukocytosis, elevated sedimentation rate, and polyclonal hypergammaglobulinemia may be observed. Approximately 40 percent of patients have extranodal involvement [4], with the skin being the most common site (11%) [5]. An infectious association has been suggested with demonstration of human herpesvirus 6 [6] and of parvovirus B19 [7] in involved tissues. Cutaneous RDD (cutaneous disease in the absence of nodal involvement) occurs in approximately 3 percent of cases of RDD [4]. There are about 80 cases reported to date [5]. Patients with cutaneous RDD may have an older age of onset, female predominance [8], and a marked Asian and white predominance [5]. Systemic complaints are generally absent with normal laboratory findings.
In a large case series, the skin lesions were divided into three main types as follows: papulonodular (79.5%), indurated plaque (12.8%), and tumor (7.7%). The extremities are the most frequently involved area followed by trunk and face [5]. Histopathologic diagnosis may present a challenge. Lesions demonstrate a dense, dermal infiltrate of typical polygonal histiocytes with scattered lymphocytes, plasma cells, and neutrophils. The histiocytes have large vesicular nuclei, small nucleoli, and abundant foamy eosinophilic cytoplasm with feathery borders. Emperipolesis (the presence of intact lymphocytes and other circulating cells within histiocytes) is common. Infiltrating histiocytes stain positively for S-100 as well as CD11c, CD14, CD68, laminin 5, and lysozyme. No Birbeck granules are present on electron microscopy [9]. Spontaneous regression tends to occur over months to years regardless of various treatments [5]. Despite recurrence in a few patients, surgical intervention remains the most effective treatment. Some patients respond to radiotherapy, cryotherapy, chemotherapy, and isotretinoin [5]. High-dose thalidomide at 300 mg daily has been reported to control extensive cutaneous disease [5, 10].
References
1. Destombes P. Adenitis with lipid excess, in children or young adults, seen in the Antilles and in Mali. (4 cases) Bull Soc Pathol Exot Filiales 1965;58:11692. Rosai J, Dorfman RF. Sinus histiocytosis with massive lymphadenopathy: a newly recognized benign clinicopathological entity. Arch Pathol 1969;87:63
3. Armitage JO, Longo DL. Malignancies of lymphoid cells. In: Braunwald E, et al. Harrison's Principles of Internal Medicine. 15th Edition. New York: McGraw Hill, 2001:721
4. Foucar E, et al. Sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease): review of the entity. Semin Diagn Pathol 1990;7:19
5. Kong YY, et al. Cutaneous Rosai-Dorfman Disease: a clinical and histopathologic study of 25 cases in China. Am J Surg Pathol 2007;31:341
6. Levine PH, et al. Detection of human herpesvirus 6 in tissues involved by sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease). J Infect Dis 1992;166:291
7. Mehraein Y, et al. Parvovirus B19 detected in Rosai-Dorfman disease in nodal and extranodal manifestations. J Clin Pathol 2006;59:1320
8. Brenn T, et al. Cutaneous rosai-dorfman disease is a distinct clinical entity. Am J Dermatopathol 2002;24:385
9. Paulli M, et al. Immunophenotypic characterization of the cell infiltrate in five cases of sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease). Hum Pathol 1992;23:647
10. Tjiu JW, et al. Cutaneous Rosai-Dorfman disease: remission with thalidomide treatment. Br J Dermatol 2003;148:1060
© 2008 Dermatology Online Journal

